In a groundbreaking study published in Nature Communications, researchers Guo, Kenmoe, Miyake, and their colleagues have provided unprecedented insights into the epidemiology of Respiratory Syncytial Virus (RSV) hospitalizations in infants, shedding light on how vulnerability changes not only with chronological age but also varies depending on the infant’s birth month. This comprehensive analysis, appearing in volume 16, article number 6109, reveals intricate patterns that have critical implications for the timing of preventive interventions, vaccine strategies, and clinical management of RSV infections, augmenting our understanding of this pervasive viral threat to infant health worldwide.
Respiratory Syncytial Virus is recognized as a leading cause of lower respiratory tract infections in infants and young children globally. The virus notoriously causes bronchiolitis and pneumonia, often resulting in hospitalizations that can overwhelm pediatric care systems each year during seasonal peaks. Despite decades of research into RSV pathogenesis and transmission dynamics, critical gaps have persisted in understanding how the risk of severe disease changes not just with the infant’s age in months but also with their month of birth, a factor linked with seasonal viral circulation patterns and possible immunological factors.
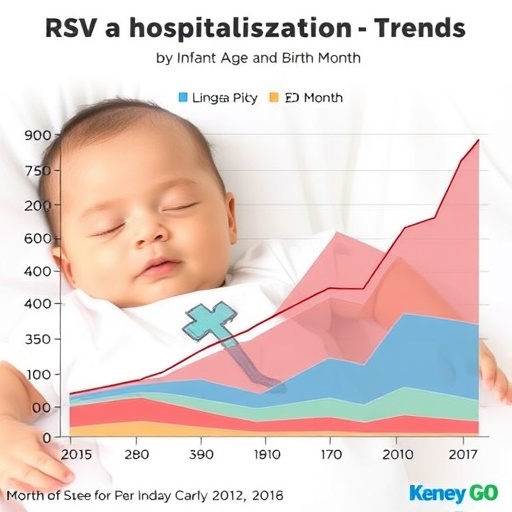
This study leverages a robust dataset encompassing hospital admissions for RSV-associated illness across multiple birth cohorts, dissecting how the risk of hospitalization evolves throughout the first months of life. The investigators applied statistical modeling that accounted for confounders such as gestational age, socioeconomic status, and underlying health conditions. Their findings reveal a nuanced interplay between chronological age and birth timing, with the highest hospitalization rates observed among infants born just before or during peak RSV season who subsequently encounter the virus at a vulnerable immunological window.
.adsslot_31lNonvAkr{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_31lNonvAkr{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_31lNonvAkr{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
One of the most compelling revelations from the study is the pronounced increase in RSV hospitalizations around the second and third months after birth, emphasizing the immature state of the neonatal immune system and its inadequate initial antibodies against RSV. Infants born in fall months, particularly September and October, faced the greatest risk since their first exposure coincided with the peak viral activity in winter, a critical period when passive maternal antibody protection wanes and infants have not yet mounted sufficient adaptive immunity.
The research team also explored immunological aspects underpinning these epidemiological patterns, discussing how maternal antibody levels transferred transplacentally decline rapidly in the first weeks postpartum, leaving a narrow window of susceptibility. This biological phenomenon aligns with epidemiological data demonstrating that infants who encounter RSV infection after this antibody decline phase are significantly more likely to develop severe disease necessitating hospitalization. Furthermore, the investigators contemplate factors such as environmental exposures, daylight variation influencing immune responses, and viral burden intensity as modifiers of disease severity linked to birth month.
In terms of public health implications, the findings present a compelling argument for optimizing prophylactic strategies like monoclonal antibody administration and emerging vaccines. Current prophylactic measures are often administered based on chronological age criteria; however, this study suggests an enhanced risk stratification approach that includes birth month as a key determinant could significantly improve target populations for intervention. For example, infants born just prior to RSV season could be prioritized for passive immunization to bridge the critical vulnerability gap in early infancy.
Importantly, the study also underscores challenges in the timing of active RSV vaccines in development. Since immunization efficacy is influenced by both the maturity of the infant immune system and the anticipated viral exposure window, understanding how protection wanes relative to birth month and seasonal viral circulation can guide scheduling to ensure maximal vaccine impact. The authors advocate for incorporating these epidemiological insights into clinical trial designs and immunization policies, potentially shifting paradigms in RSV prevention.
From a virological perspective, the research further contributes to understanding RSV seasonality. The virus is characterized by pronounced annual peaks, often in the cold months in temperate climates, driven by factors including indoor crowding, humidity, and virus stability in the environment. By analyzing hospitalizations aligned to infant birth months, the authors uniquely correlate individual exposure timing with population-level viral transmission dynamics, highlighting the importance of synchronizing intervention timing with epidemiological trends.
Moreover, the methodology utilized is notable for integrating multi-layered data—a first in RSV hospitalization studies. Combining individual-level clinical data with temporal birth cohorts and robust statistical modeling allowed the researchers to control for biases such as varying healthcare-seeking behavior and surveillance intensity across seasons. Their approach sets a new standard for respiratory virus epidemiology research, providing a template for studying other pathogens with seasonal behavior patterns.
Beyond immediate clinical ramifications, the data yield insights into the biological and environmental determinants of infant immunity. The intersection of age-related immune system maturation and seasonal external factors—ranging from viral prevalence to ambient temperature—underscore the complexity underlying respiratory infection risk. These findings invite further mechanistic studies exploring how seasonally modulated immune ontogeny and exposure history influence susceptibility to RSV and subsequent immune memory formation.
The study also touches on the implications for health equity and resource allocation. In many regions, RSV imposes a disproportionate burden on vulnerable populations, often linked to socioeconomic factors that affect healthcare access and environmental exposures. The researchers note that birth month-based risk stratification could enable more precise allocation of limited prophylactic resources to those infants most at risk, potentially reducing disparities in RSV-associated morbidity and mortality.
Overall, the extensive data and rigorous analyses presented offer a transformative understanding of RSV infection risk that transcends simplistic age-based categories. By illuminating how birth month confers differential vulnerability mediated through complex immunological and environmental mechanisms, the study equips clinicians, public health officials, and vaccine developers with refined knowledge to craft tailored prevention strategies. As RSV remains a formidable challenge globally, advancements derived from such comprehensive research are essential in moving toward effective and equitable control of this ubiquitous pediatric pathogen.
The publication’s multidisciplinary authorship team, combining expertise in virology, immunology, pediatrics, and epidemiology, underscores the collaborative nature required for tackling intricate infectious disease questions. Their work exemplifies how large-scale data analysis coupled with biological insight can reveal subtle but critical determinants of disease risk, ultimately informing interventions that save lives and optimize healthcare delivery in vulnerable infant populations.
As efforts accelerate globally toward RSV vaccines and novel therapeutics, the implications of this study resonate profoundly. It advises a reconsideration of existing prophylaxis frameworks, urging stakeholders to incorporate nuanced risk factors beyond simple age cutoffs, thereby enhancing the precision and effectiveness of interventions. The research thereby lays the groundwork for dynamic prevention paradigms sensitive to temporal and biological contexts that characterize RSV infection in early life.
In conclusion, this landmark study expands the frontiers of RSV epidemiology by demonstrating how chronological age and birth month jointly dictate hospitalization risk in infants. It challenges existing paradigms and establishes evidence-based directives for personalized approaches to RSV prevention, with profound potential to reduce infant morbidity and mortality worldwide. Such insights are pivotal at a time when RSV remains a critical public health concern despite ongoing vaccine development efforts, underscoring the continual need for in-depth investigation into the complex factors influencing infectious disease outcomes.
Subject of Research:
Hospitalization patterns of Respiratory Syncytial Virus in infants analyzed by chronological age and birth month.
Article Title:
Respiratory syncytial virus hospitalisation by chronological month of age and by birth month in infants.
Article References:
Guo, L., Kenmoe, S., Miyake, F. et al. Respiratory syncytial virus hospitalisation by chronological month of age and by birth month in infants. Nat Commun 16, 6109 (2025). https://doi.org/10.1038/s41467-025-61400-1
Image Credits:
AI Generated
Tags: bronchiolitis and pneumonia in infantsclinical management of RSV infectionsimmunological factors in RSVinfant age and birth monthinfant health and viral infectionslongitudinal study of RSV hospitalizationspediatric care system overloadrespiratory syncytial virus epidemiologyRSV hospitalization trendsRSV preventive interventionsseasonal patterns of RSVvaccine strategies for RSV