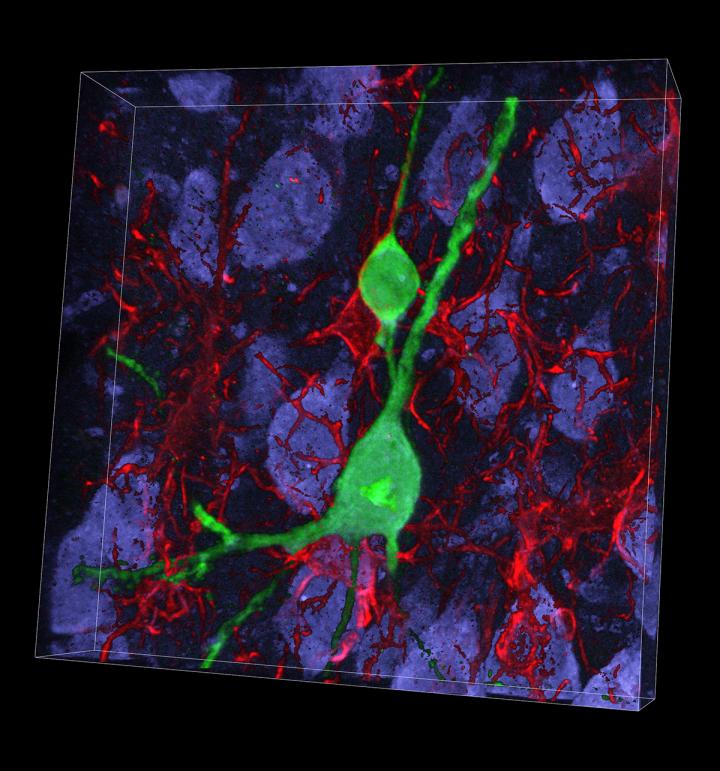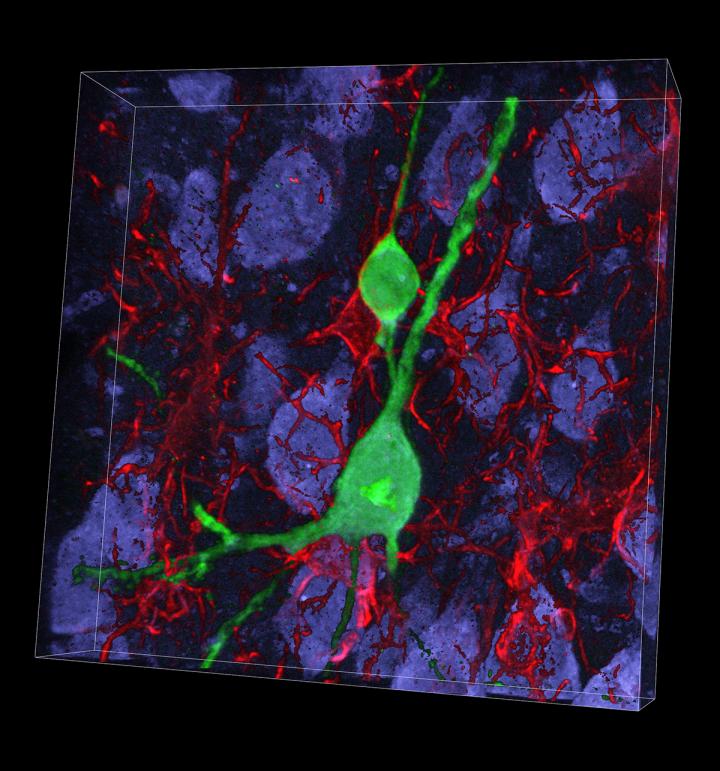
Credit: Rosalind Franklin University
A $2.8 million grant from the National Institutes of Health (NIH) will help researchers at Rosalind Franklin University of Medicine and Science study how to replace neurons lost through stroke, traumatic brain and spinal injury and brain diseases including Alzheimer's.
The five-year grant was recently awarded to Daniel A. Peterson, Ph.D., director of the university's Center for Stem Cell and Regenerative Medicine, and Robert Marr, Ph.D., Chicago Medical School associate professor of neuroscience, for the study "Reprogramming Cell Fate for Repair," a collaboration with co-principal investigators Oliver Brüstle, M.D., and Martin Schwarz, Ph.D., at the University of Bonn in Germany.
"Our new reprogramming technology allows us to try to make neurons wherever they're needed in the brain for repair and we're having some success," Dr. Peterson said. "What we're still trying to figure out is how to make enough of them and how to make them connect with the existing circuit."
Brain and Spinal Cord Repair
Neurons in the brain and spinal cord are long-lived cells that are not replaced when damaged or lost. Recent advances in stem cell biology make it possible to introduce developmental genes into mature cells and direct them to change their fate by becoming a different type of cell. The study will use gene therapy approaches to directly reprogram rodent and human progenitor cells, which descend from stem cells to become neurons, and then evaluate the extent to which these newly engineered neurons connect with the rest of the brain. The findings could lead to new therapies for neurological injury and disease such as stroke, spinal cord injury, and traumatic brain injury (TBI) — a long-term focus of the project.
At present, there are few options to repair neurons lost through injuries such as stroke or TBI or neurodegenerative diseases such as Alzheimer's or Parkinson's diseases, or amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig's disease. According to the Centers for Disease Control, an estimated 1.7 million people per year suffer a TBI, many of whom incur permanent disability as a result. Mild TBI is one of the most common neurologic disorders accounting for approximately 90 percent of all brain injuries sustained. Such injuries are a common occurrence in athletes. Sport-related concussions number an estimated 2 to 4 million annually in the U.S.
Dr. Peterson's team, which has also included researchers at DePaul University in Chicago, is investigating neuronal loss in an animal model of mild TBI with the goal of applying the reprogramming approach to replace lost neurons and restore function.
Collaboration with University of Bonn
The NIH award to Dr. Peterson originated from his successful proposal for the Fulbright Senior Scholar Award, which supported his year as a visiting professor at the University of Bonn, Germany. His work with researchers there led to innovations and initial data that helped form the direction of a continued collaboration and the framework for the NIH grant. The sabbatical year yielded two scientific publications, including co-authorship on a paper in Nature Communications entitled "Whole-brain 3D mapping of human neural transplant innervation".
"Programs like the Fulbright Scholar Program and the Council for International Exchange of Scholars (CIES) sponsored by the U.S. Department of State are important for maintaining important connections and realizing the value of international cooperation," Dr. Peterson said. "I hope our grant through NIH further supports those international ties. We have more in common than divides us."
In Germany, Dr. Peterson worked closely with Drs. Brüstle and Schwarz, leading experts in stem cell biology and neural circuitry, respectively. Dr. Brüstle is also director of the University of Bonn's Institute of Reconstructive Neurobiology, part of the university's Life & Brain Center, its translation hub and a key contributor to translational science in the German State of North Rhine Westphalia. The IRN participates in a number of national and European research consortia, including the 7 FP project Neurostemcellrepair, the Horizon 2020 project COSYN and several consortia of the Innovative Medicines Initiative.
"This NIH award and the Fulbright Award-supported sabbatical that established the collaborative project, is a wonderful example of how government investment can help scientists extend their research in new directions," said Ronald Kaplan, Ph.D., RFU executive vice president for research. "The grant will support new discoveries by Dr. Peterson and his team with one goal in mind: improved health and well-being."
###
About Rosalind Franklin University of Medicine and Science
Formed in 1912 as the Chicago Hospital-College of Medicine, Rosalind Franklin University of Medicine and Science is a national leader in interprofessional medical and healthcare education and biomedical research. RFU includes the Chicago Medical School, School of Graduate and Postdoctoral Studies, College of Health Professions, Dr. William M. Scholl College of Podiatric Medicine and College of Pharmacy. More than 18,000 RFU degreed alumni are active throughout the United States and around the world. Learn more at rosalindfranklin.edu.
Media Contact
Judith Masterson
[email protected]
847-578-8313
@RFUniversity
http://www.rosalindfranklin.edu