A comprehensive new study led by researchers at Columbia University projects a significant and troubling rise in the incidence and mortality of uterine cancer in the United States over the next 25 to 30 years. This analysis, grounded in sophisticated natural history modeling, indicates that the burden of uterine cancer is set to increase disproportionately among Black women compared to their white counterparts. These findings highlight urgent public health challenges regarding prevention, diagnosis, and treatment strategies tailored to high-risk populations, especially given that uterine cancer remains one of the few malignancies with climbing incidence and mortality rates nationally.
Uterine cancer rates have surged dramatically in recent years. Epidemiological data demonstrate that between 2010 and 2020, new uterine cancer cases increased by over 50%, jumping from approximately 43,000 to more than 65,000 diagnosed cases annually. This upward trajectory is particularly alarming, as it threatens to exacerbate existing racial disparities wherein mortality rates are currently estimated to be twice as high among Black women than among white women. This steep increase underscores the complexity of factors fueling the epidemic and the inadequacy of current interventions.
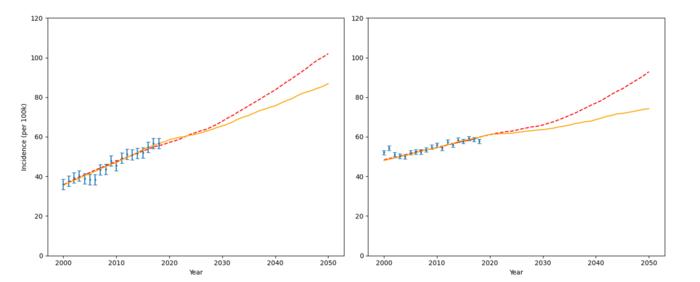
At the core of the Columbia study is the development and utilization of a detailed natural history simulation model that accounts for multiple intersecting variables influencing uterine cancer risk and outcomes. This model incorporated age-specific data, histologic subtypes of uterine cancer, racial demographics, obesity rates, and hysterectomy prevalence, offering a nuanced projection of disease trends through 2050. By simulating women’s health trajectories over time, the researchers could examine how shifts in obesity and surgical intervention rates might influence future disease dynamics under different scenarios.
.adsslot_ALfHstCxz6{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_ALfHstCxz6{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_ALfHstCxz6{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Obesity is a well-established key driver of uterine cancer risk, principally due to its role in hormonal dysregulation, including elevated estrogen levels, which promote endometrial carcinoma development. Meanwhile, hysterectomy rates, which effectively remove the uterus and eliminate the risk of uterine cancer, have been declining, particularly among younger women. These contrasting trends—rising obesity and falling hysterectomy rates—serve as pivotal variables in the model, as their trajectories critically impact the predicted incidence rates for uterine cancer.
The projections indicate a stark racial disparity in disease burden. From 2018 to 2050, the model forecasts an increase in uterine cancer cases exceeding 50% among Black women, whereas white women are expected to experience a more modest rise of approximately 29%. This disparity likely reflects a confluence of biological, socioeconomic, and health system factors. For example, tumors in Black women tend to be diagnosed at more advanced stages and demonstrate more aggressive histologic types, leading to poorer prognoses. Additionally, systemic barriers contribute to delays in diagnosis and treatment initiation.
A consistent theme emerging from the study is the urgent need to enhance uterine cancer screening and early detection efforts. Current standard diagnostic methods, such as transvaginal ultrasound and endometrial biopsy, primarily target symptomatic individuals, typically those presenting with abnormal uterine bleeding. This reactive approach misses opportunities for early intervention in asymptomatic women, who may carry undetected precancerous changes. The study’s simulation model tested hypothetical screening strategies, revealing that introduction of effective screening starting at age 55 could substantially curtail uterine cancer incidence.
Emerging liquid biopsy technologies offer promise as potential screening tools for uterine cancer. These innovative assays detect circulating tumor DNA and other cellular markers shed into bodily fluids, enabling non-invasive identification of precancerous or early malignant changes within the uterus. If validated for clinical use, such diagnostics could revolutionize early detection paradigms and mitigate mortality among high-risk populations. However, translating these advances into practice will require overcoming substantial challenges related to sensitivity, specificity, and accessibility.
The study’s multidisciplinary authorship spans leading academic institutions and national research bodies, reflecting the collaborative effort required to address this complex public health threat. By leveraging robust epidemiological data combined with computational modeling, the research delineates actionable insights into the trajectory of uterine cancer and underscores the disproportionate impact on Black women. Enhanced awareness and targeted intervention strategies rooted in this knowledge can guide policy and clinical practice.
Concurrently, the research acknowledges the role that social determinants of health play in amplifying racial disparities in uterine cancer outcomes. Factors such as access to care, socioeconomic status, health literacy, and bias within healthcare systems compound biological risk to produce inequities in incidence and survival. Tackling uterine cancer effectively thus demands holistic approaches that integrate medical innovation with systemic changes aimed at equity.
Importantly, the study was supported by funding from the National Institutes of Health, underscoring the federal commitment to understanding and combating gynecologic cancers. Transparency regarding potential conflicts of interest was maintained, with disclosed relationships between certain authors and pharmaceutical or professional entities ensuring scientific integrity. This commitment bolsters confidence in the study’s conclusions and their implications for future research priorities.
Looking ahead, the findings urge clinicians, researchers, and public health officials to prioritize uterine cancer as a rising threat requiring innovative prevention, screening, and treatment modalities. Development of effective screening tests, public health campaigns targeted at obesity reduction, and interventions addressing healthcare disparities are critical components of a comprehensive response. Without concerted action, the projected increases in uterine cancer will place mounting strain on patients, families, and healthcare systems alike.
In conclusion, this landmark study offers a detailed forecast of uterine cancer’s disturbing ascent in the United States, particularly among Black women disproportionately affected by its morbidity and mortality. Through advanced modeling and careful epidemiological analysis, it provides an indispensable roadmap for addressing a cancer that has, until recently, received comparatively limited attention. The imperative is clear: to stem this tide through innovation, equity, and dedicated public health efforts.
Subject of Research: Projected incidence and mortality trends of uterine cancer in the United States with focus on racial disparities
Article Title: Projected Trends in the Incidence and Mortality of Uterine Cancer in the United States
News Publication Date: July 1, 2025
Web References:
DOI Link
Image Credits: Columbia University Irving Medical Center
Keywords: Uterine cancer, cancer epidemiology, racial disparities, obesity, hysterectomy, cancer screening, liquid biopsy, natural history model
Tags: Black women health issuescancer prevention strategiesColumbia University cancer researchdiagnosis of uterine cancerepidemiological trends in cancerhealth disparities in cancernatural history modeling in cancer researchpublic health challenges in cancerracial disparities in healthcarerising uterine cancer mortalitytreatment approaches for uterine canceruterine cancer incidence rates