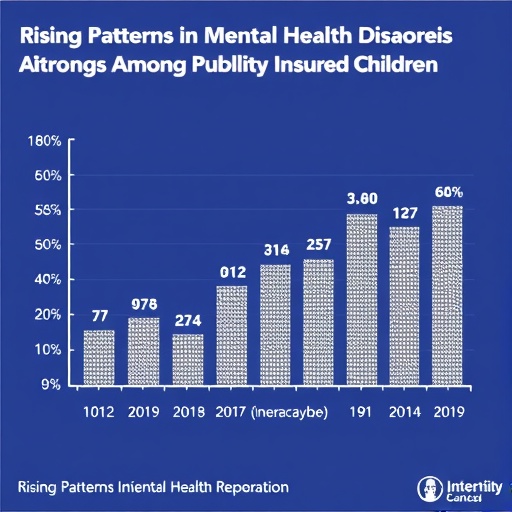
Over the past decade, the mental health landscape for publicly insured children in the United States has undergone a significant transformation. An extensive study reveals a marked increase in the percentage of these children receiving diagnoses related to mental health conditions or neurodevelopmental disorders between 2010 and 2019. This surge is not limited to a few isolated conditions but spans across most diagnostic categories examined in the analysis, indicating a broad shift in either recognition, reporting, or actual incidence rates of these disorders within this demographic group.
This upward trend brings to the forefront critical implications for public health infrastructure, especially the safety net systems that predominantly serve publicly insured populations. These systems, often resource-constrained, must grapple with growing demands for specialized mental health services and supports. The findings urge policymakers, healthcare providers, and community stakeholders to revisit and reinforce the structural capacities necessary to meet this rising clinical need adequately.
To understand the nuances underlying this development, it is crucial to contextualize the increased diagnosis rates within broader societal and healthcare changes over the decade. Enhanced awareness of mental health issues, destigmatization efforts, and evolving diagnostic criteria might have contributed to greater identification of these disorders. Simultaneously, advances in screening techniques and access to care, though uneven, may have improved detection, especially within publicly insured populations who historically faced barriers in service utilization.
However, attributing the rise solely to diagnostic improvements or detection biases would be reductive. There may be genuine increases in incidence driven by environmental, social, and economic stressors disproportionately affecting low-income families who constitute the majority of publicly insured children. Factors such as community violence, housing instability, food insecurity, and educational disruptions can exacerbate vulnerabilities to mental health challenges, thus reflecting in higher diagnosis rates documented in the study.
The research also sheds light on the heterogeneity of diagnostic trends across different mental health and neurodevelopmental disorders. While the study did not elaborate exhaustively on each category, the general pattern suggests that conditions such as attention-deficit/hyperactivity disorder (ADHD), anxiety disorders, depressive disorders, and autism spectrum disorders are key contributors to the observed increases. This calls for a granular exploration into how each disorder’s prevalence and recognition have evolved amidst shifting healthcare policies and practices.
This changing epidemiological profile posits serious questions about service availability and quality. The capacity of safety net providers, including community mental health centers, school-based services, and pediatric clinics, must be calibrated to accommodate this burgeoning population of children with complex mental health needs. Integrated care models that combine physical and mental health services within primary care settings could serve as a vital strategy in enhancing accessibility and continuity of care for publicly insured youth.
Moreover, the study’s findings underscore the significance of health insurance coverage as a determinant of access to mental health diagnosis and care. Public insurance programs, primarily Medicaid and the Children’s Health Insurance Program (CHIP), play an indispensable role in enabling families to seek and receive mental health evaluations. Strengthening these programs, both in funding and scope, is essential to ensuring that increasing diagnostic trends translate into effective treatment rather than unaddressed morbidity.
The research further highlights the critical need for targeted workforce development in child mental health specialties. The increasing caseloads necessitate a robust cadre of child psychiatrists, psychologists, social workers, and behavioral health specialists trained to address the unique challenges faced by children under public insurance. Training programs and incentives should be designed to attract professionals to underserved areas where the need is often greatest.
In parallel, the amplification of telehealth services represents a promising avenue to bridge gaps in mental health service delivery. Especially in the wake of widespread disruptions caused by the COVID-19 pandemic, virtual care has gained traction and could continue to be leveraged to reach children who face logistical or geographic barriers to in-person visits. Policymakers and healthcare systems must contemplate sustainable models that integrate telepsychiatry within the broader public health framework.
Importantly, the study accentuates the intersection of mental health diagnosis with broader demographic and socioeconomic factors. Disparities related to race, ethnicity, and socio-economic status intersect with insurance type to influence diagnosis rates and access to services. Tailored interventions that address these disparities holistically are integral to realizing equitable mental health outcomes for all children.
Finally, these revelations prompt an urgent call for ongoing research to elucidate the drivers of increased mental health and neurodevelopmental disorder diagnoses among publicly insured children. Longitudinal studies exploring causal relationships, the impact of policy changes, and the effectiveness of intervention programs will be pivotal in crafting evidence-based strategies that can turn diagnostic increases into positive therapeutic engagements and ultimately, improved child wellbeing.
In summary, the decade-long rise in mental health and neurodevelopmental disorder diagnoses within the publicly insured pediatric population signals a multifaceted phenomenon with profound implications. It simultaneously illuminates progress in recognition and invites scrutiny of persistent and emerging challenges in service delivery, equity, and health system capacity. Addressing these complexities decisively will require concerted efforts across clinical, policy, and community domains.
Subject of Research: Trends in Mental Health and Neurodevelopmental Disorder Diagnoses Among Publicly Insured Children
Article Title: Not provided
Keywords: Mental health, Psychiatric disorders, Medical diagnosis, Public health, Children, Population, Health insurance
Tags: children’s mental health supportdestigmatization of mental health issuesdiagnostic criteria evolutionhealthcare system challengesincrease in mental health awarenessmental health diagnoses in childrenmental health services demandneurodevelopmental disorders trendspublic health implications for mental healthpublic policy for mental health carepublicly insured children mental healthsocietal changes in mental health recognition