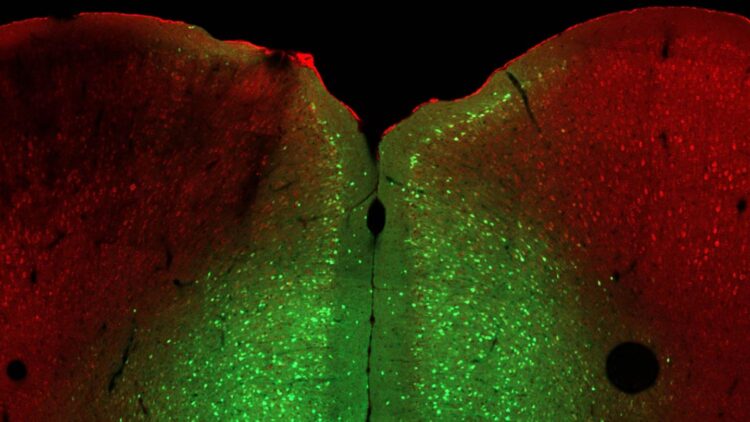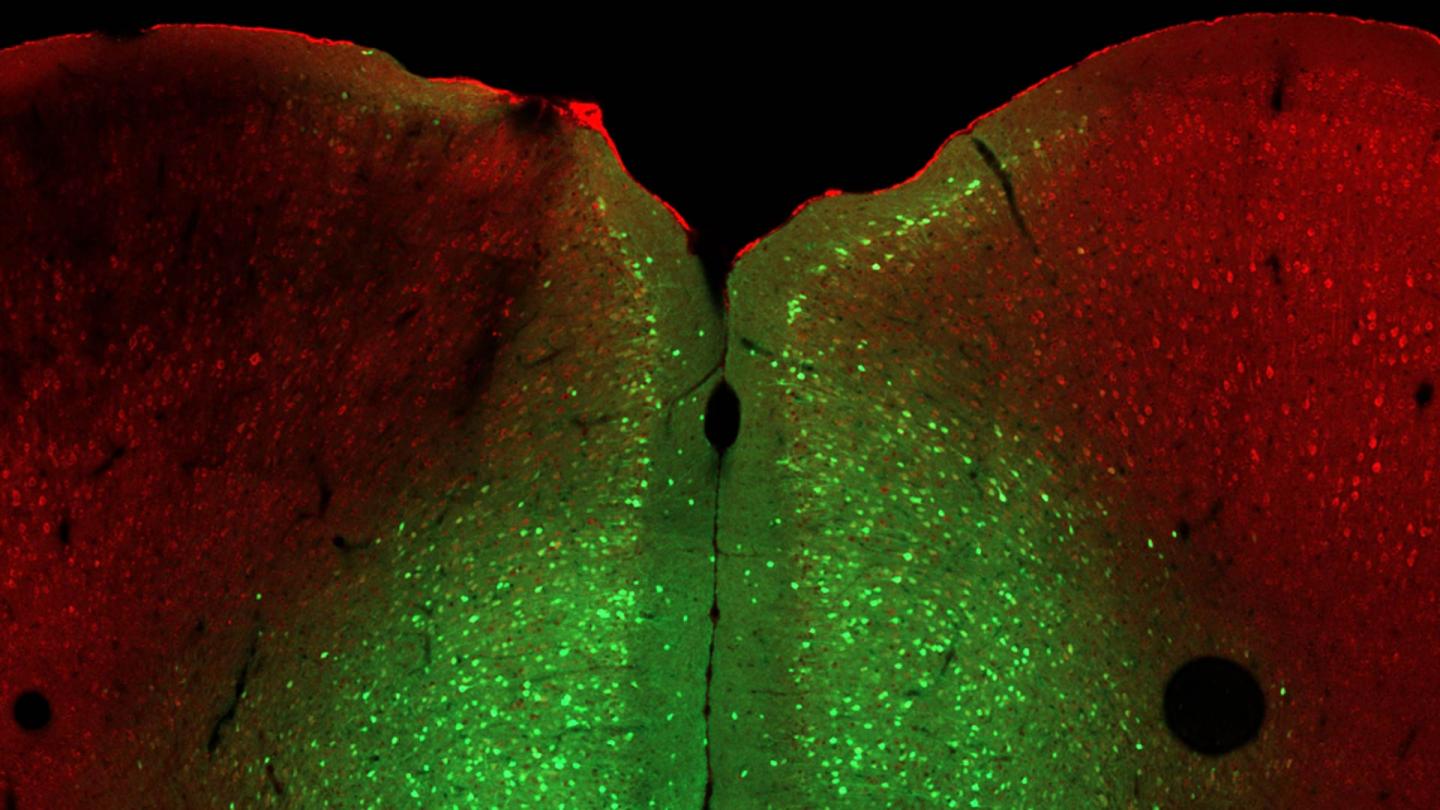
Credit: Minghui Wang/Van Aelst Lab, CSHL/2021
Everyone faces stress occasionally, whether in school, at work, or during a global pandemic. However, some cannot cope as well as others. In a few cases, the cause is genetic. In humans, mutations in the OPHN1 gene cause a rare X-linked disease that includes poor stress tolerance. Cold Spring Harbor Laboratory (CSHL) Professor Linda Van Aelst seeks to understand factors that cause specific individuals to respond poorly to stress. She and her lab studied the mouse gene Ophn1, an analog of the human gene, which plays a critical role in developing brain cell connections, memories, and stress tolerance. When Ophn1 was removed in a specific part of the brain, mice expressed depression-like helpless behaviors. The researchers found three ways to reverse this effect.
To test for stress, the researchers put mice into a two-room cage with a door in between. Normal mice escape from the room that gives them a light shock on their feet. But animals lacking Ophn1 sit helplessly in that room without trying to leave. Van Aelst wanted to figure out why.
Her lab developed a way to delete the Ophn1 gene in different brain regions. They found that removing Ophn1 from the prelimbic region of the medial prefrontal cortex (mPFC), an area known to influence behavioral responses and emotion, induced the helpless phenotype. Then the team figured out which brain circuit was disrupted by deleting Ophn1, creating overactivity in the brain region and ultimately the helpless phenotype.
Understanding the circuit
Pyramidal neurons are central to this brain circuit. If they fire too much, the mouse becomes helpless.
Another cell, an interneuron, regulates the pyramidal neuron activity, making sure it does not fire too much.
These two cells feedback to each other, creating a loop.
Ophn1 controls a particular protein, RhoA kinase, within this feedback loop which helps regulate and balances activity.
Van Aelst found three agents that reversed the helpless phenotype. Fasudil, an inhibitor specific for RhoA kinase, mimicked the effect of the missing Ophn1. A second drug dampens excess pyramidal neuron activity. A third drug wakes up the interneurons to inhibit pyramidal neurons. Van Aelst says:
“So bottom line, if you can restore the proper activity in the medial prefrontal cortex, then you could rescue the phenotype. So that was actually very exciting. You should be open to anything. You never know. Everything is surprising.”
Van Aelst hopes that understanding the complex feedback loop behind Ophn1-related stress responses will lead to better treatments for stress in humans.
###
Media Contact
Sara Roncero-Menendez
[email protected]
Related Journal Article
http://dx.