Study could pave the way for future targeted treatments for kidney disease
Credit: University of Maryland School of Medicine
Researchers from the Center for Precision Disease Modeling at the University of Maryland School of Medicine (UMSOM) have uncovered a mechanism that appears to explain how certain genetic mutations give rise to a rare genetic kidney disorder called nephrotic syndrome. Using a drosophila (fruit fly) model, they found mutations in genes that code for certain proteins lead to a disruption of the recycling of the cell membrane. This disruption leads to an abnormal kidney cell structure and function, according to the study published this week in the Journal of the American Society of Nephrology.
Disruption of kidney cell function leads to nephrotic syndrome, a kidney disease that causes an abnormal amount of protein leaking into the urine due to a problem with the kidney’s filters. It occurs in about 7 in 100,000 Americans, and though rare, it is considered one of the most common kidney diseases in children. Nephrotic syndrome caused by genetic mutations often does not respond to the standard steroid treatment, so treatment depends on the identification of the genetic mutation that causes the disease, followed by targeted therapeutic development based on the disease mechanism. There are, however, no known treatments for the condition when it is caused by mutations in the genes examined in this study.
“Researchers have recently identified a mutation in one of the genes that codes for these proteins, called the exocyst complex, that has been linked to kidney disease,” says Zhe Han, Ph.D., Associate Professor at the Department of Medicine and Director of the Center for Precision Disease Modeling at UMSOM. “However, the underlying mechanism by which the exocyst complex contributes to kidney disease had long been a mystery.”
Dr. Han’s team used Drosophila as a model to better understand the mechanism by which these gene mutations potentially give rise to kidney disease. Drosophila have specialized filtration cells (nephrocytes) that closely resemble human podocytes, a type of kidney cell associated with nephrotic syndrome, both in structure and function. Using the power of fly genetics, the research team carried out a genetic screen with Drosophila and identified each of the eight exocyst genes that are required for nephrocytes to function properly.
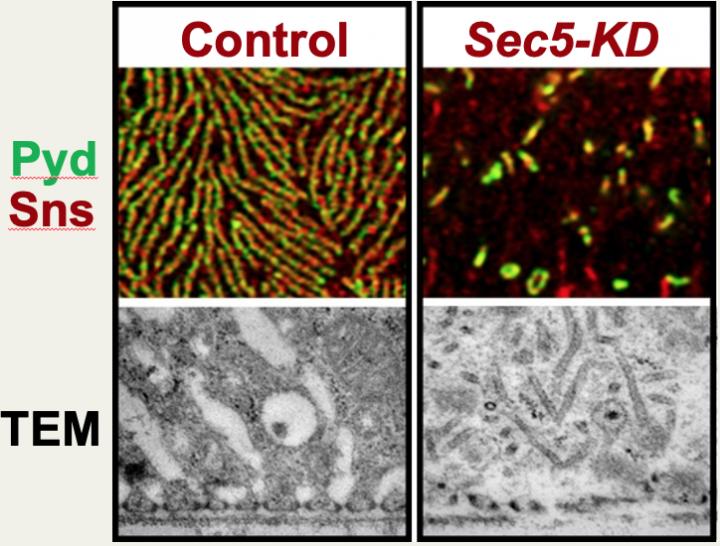
Silencing the Drosophila exocyst genes in nephrocytes led to a disruption of a structure essential for filtering called the nephrocyte slit diaphragm. The researchers then used a transmission electron microscope to take a closer look at the ultrastructural changes, which revealed the appearance of unique electron-dense tubular structures which they named “exocyst rods”.
“Therefore, the formation of the exocyst rods can be used as a new biomarker for diseases caused by genetic mutations in exocyst genes,” Dr. Han said.
The finding, if replicated, also has important clinical implications for patients who are screened for genetic kidney diseases. “Our study suggests that mutations in all eight exocyst genes could lead to nephrotic syndrome and thus should be included in the sequencing panel for genetic kidney diseases,” Dr. Han said.
Dr. Han and his team are currently using their Drosophila model to gain additional insight into the mechanisms regulating slit diaphragm proteins and how their disruption might contribute to the podocyte pathogenesis seen in kidney disease patients.
“This is an important finding that demonstrates the important mission of the Center for Precision Disease Modeling at the University of Maryland School of Medicine,” said UMSOM Dean E. Albert Reece, MD, PhD, MBA, who is also the Executive Vice President for Medical Affairs, University of Maryland, and the John Z. and Akiko K. Bowers Distinguished Professor. “Further studies to understand this molecular mechanism could lead to a new targeted therapeutic approach that could eventually benefit patients with this devastating kidney disease.”
###
The research was funded by the National Institutes of Health.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world — with 45 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has more than $540 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 student trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of nearly $6 billion and an economic impact more than $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th highest among public medical schools in research productivity, is an innovator in translational medicine, with 600 active patents and 24 start-up companies. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Media Contact
Deborah Kotz
[email protected]
Original Source
https:/




