Credit: Hong et al., 2019
A study of pregnant women with systemic lupus erythematosus has identified early changes in the RNA molecules present in the blood that could be used to determine the likelihood of them developing preeclampsia. The study, which will be published April 8 in the Journal of Experimental Medicine, may also help researchers develop treatments to prevent other pregnancy complications associated with lupus, including miscarriage and premature birth.
Lupus is an autoimmune disease in which the immune system attacks the body’s own healthy tissues. The disease predominantly affects women and carries an increased risk of developing complications during pregnancy; approximately one fifth of pregnant lupus patients develop problems ranging from preeclampsia to fetal death and preterm delivery.
“Early biomarkers are needed to help predict pregnancy outcome and inform treatments to decrease morbidity and mortality in lupus pregnancies,” says co-senior author Virginia Pascual, the Drukier Director of the Drukier Institute for Children’s Health at Weill Cornell Medicine in New York. To address this problem, Dr. Pascual teamed up with Dr. Jane E. Salmon, a Professor of Medicine and of Medicine in Obstetrics and Gynecology at Weill Cornell Medicine, and the Collette Kean Research Professor at the Hospital for Special Surgery in New York. Dr. Salmon and her team recruited healthy and lupus pregnant women as part of the PROMISSE study, a longitudinal NIH-funded study aimed at identifying biomarkers of lupus pregnancy complications.
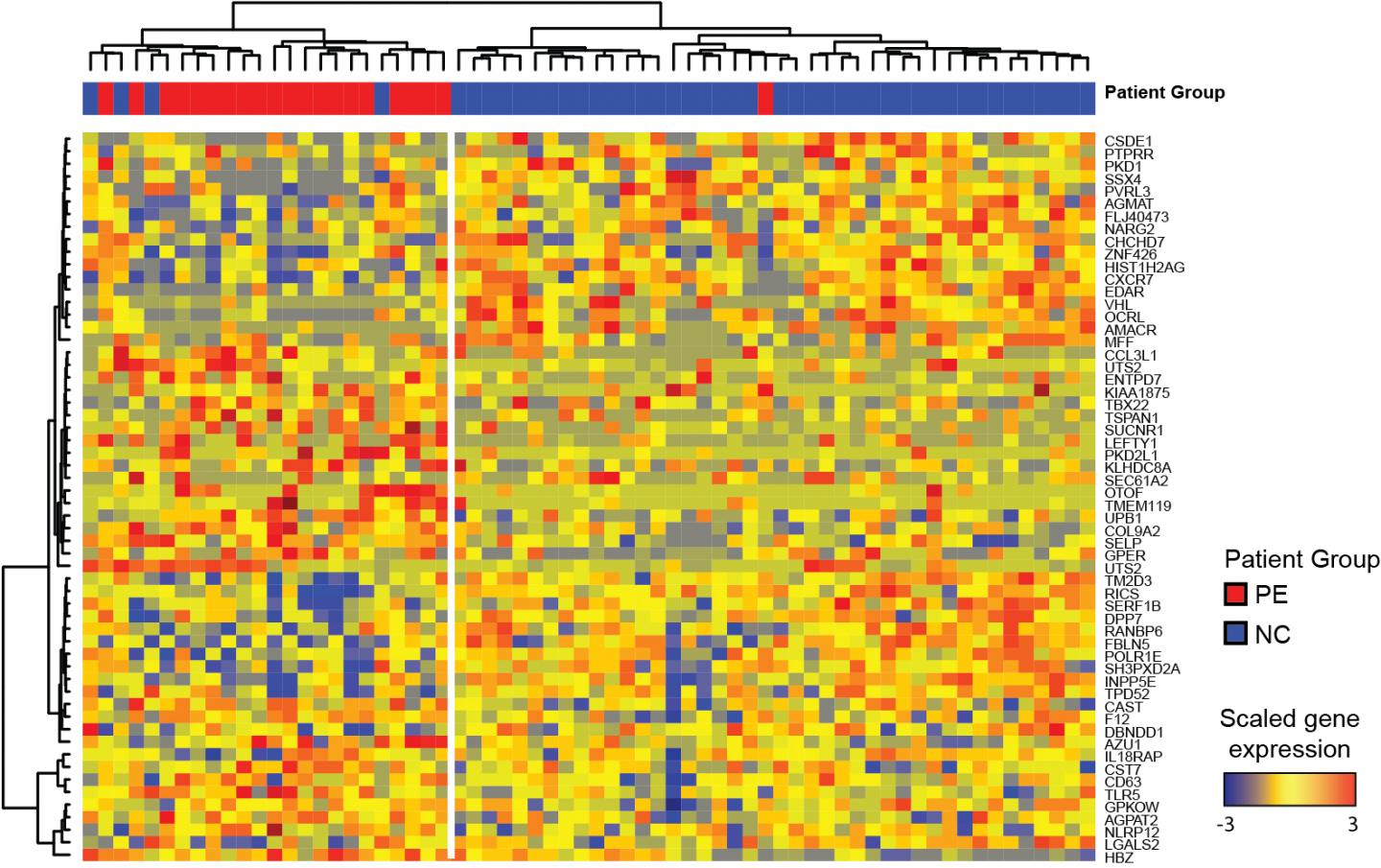
To identify potential biomarkers, Pascual, Salmon, and colleagues compared blood samples taken at regular intervals from either pregnant lupus patients or healthy pregnant women. The researchers counted the different types of immune cells present in these samples and, as a measure of which genes were active in these cells, analyzed the RNA molecules they produced over the course of pregnancy and in the postpartum period.
In a healthy pregnancy, the immune system is prevented from attacking the developing fetus. Accordingly, Pascual, Salmon, and colleagues found that several components of the immune system, including antibody-producing plasma cells and the proinflammatory interferon response, were suppressed in healthy pregnant women. An additional analysis of women undergoing assisted reproductive therapy suggested that the interferon response, in particular, is downregulated within days of embryo implantation. At later stages of pregnancy, however, some components of the immune system, such as the number of neutrophil cells, were elevated in healthy pregnant women.
Pascual, Salmon, and colleagues found that lupus patients with uncomplicated pregnancies showed similar changes in their immune systems. However, neutrophil levels increased earlier than normal in patients that developed preeclampsia. By analyzing the RNAs present in the blood of these patients during early pregnancy, the researchers were able to identify a unique immune signature that could predict the development of preeclampsia more accurately than existing clinical factors.
“Our results need to be independently validated, but they suggest that early changes in gene expression in maternal blood could help predict preeclampsia in lupus patients,” Salmon, co-senior author, says.
In addition, the researchers found that patients who developed other complications failed to properly suppress their interferon response and plasma cell activity.
“Overall, we have identified significant changes in immune pathways during healthy pregnancy and found that failure to modulate them properly is associated with complications in pregnant lupus patients,” Pascual says. “Our findings provide a framework for future studies aimed at developing therapeutic strategies to improve health outcomes for mothers with lupus and their offspring.”
Dr. Pascual has received a research grant and consulting honorarium from Sanofi-Pasteur. Dr. Salmon has received an investigator-initiated grant from UCB Pharmaceuticals.
###
Hong et al., 2019. J. Exp. Med. http://jem.
About the Journal of Experimental Medicine
The Journal of Experimental Medicine (JEM) features peer-reviewed research on immunology, cancer biology, stem cell biology, microbial pathogenesis, vascular biology, and neurobiology. All editorial decisions are made by research-active scientists in conjunction with in-house scientific editors. JEM makes all of its content free online no later than six months after publication. Established in 1896, JEM is published by Rockefeller University Press. For more information, visit jem.org.
Visit our Newsroom, and sign up for a weekly preview of articles to be published. Embargoed media alerts are for journalists only.
Follow JEM on Twitter at @JExpMed and @RockUPress.
Media Contact
Ben Short
[email protected]
Related Journal Article
http://dx.




