There’s a tried and proven pathway to reducing racial disparities in cancer in Delaware. It worked with colon cancer 10 years ago and should now be applied to the incidence of breast cancer in the state. That’s the recommendation of clinicians, program leaders and researchers from the ChristianaCare Helen F. Graham Cancer Center & Research Institute in a new commentary published in Population Health Management on Nov. 1, 2023.
Credit: ChristianaCare
There’s a tried and proven pathway to reducing racial disparities in cancer in Delaware. It worked with colon cancer 10 years ago and should now be applied to the incidence of breast cancer in the state. That’s the recommendation of clinicians, program leaders and researchers from the ChristianaCare Helen F. Graham Cancer Center & Research Institute in a new commentary published in Population Health Management on Nov. 1, 2023.
The commentary — “Reducing Racial Disparities in Breast Cancer: Getting the Village Back Together” — is a call to action for community members, health care providers and other stakeholders to partner together to address disparities in breast cancer.
“Breast cancer is the leading cause of cancer deaths for Black women in the United States,” said Scott Siegel, Ph.D., MHCDS, director of Cancer Control & Population Sciences at ChristianaCare and the paper’s lead author. “We see more occurrences in communities that bear the impacts of structural racism, including historical redlining and a lack of access to affordable housing, equitable health care, fair financial services and environmental safeguards. Other risk factors, which also can be directly or indirectly related to entrenched racism, are limited breastfeeding, obesity, diabetes and alcohol use.”
‘Alarming disparities’
Although Black and white women are diagnosed with breast cancer at similar rates, Black women experience a 40% higher mortality rate. This disparity appears to be driven by a much higher mortality rate for Black women under 50, who are at an 18% greater risk of being diagnosed with advanced breast cancer than white women of the same age. Black women younger than 50 also have an 88% higher risk of dying from advanced breast cancer than white women.
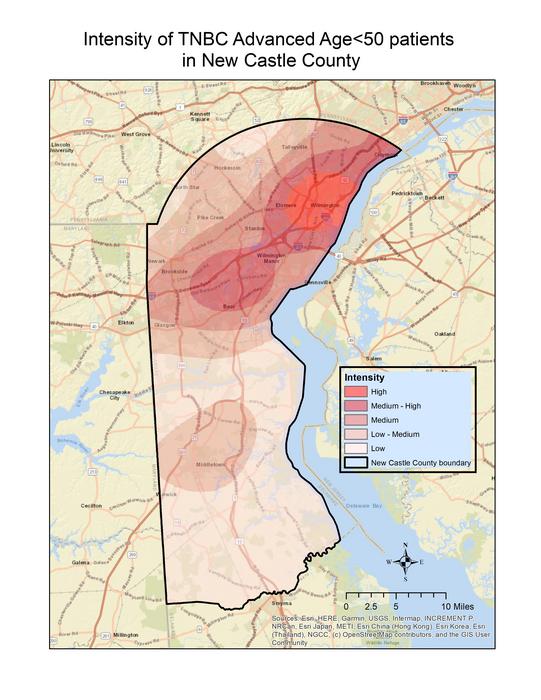
More than half of this difference is attributed to triple-negative breast cancer (TNBC). This aggressive cancer appears at a younger age and is twice as prevalent among Black women.
According to the National Cancer Institute, Delaware leads the country in incidences of late-stage breast cancer among women younger than 50. The state also leads nationwide in rates of TNBC among Black women and has the largest racial disparity in TNBC incidences.
“Living without opportunities and resources critical to thriving communities threatens women’s breast health,” said Siegel. “We are excited at the possibility of bringing the larger village back together again to tackle the disparities in breast cancer. And, while our commentary focuses on racial disparities, the plan also stands to benefit other groups who experience poor breast cancer outcomes, including Latino, Ashkenazi Jewish and transgender individuals.”
Two-pronged approach to success
Siegel and his ChristianaCare coauthors present two strategies for reducing breast cancer occurrence and mortality rates:
- Advising women statewide to get regular mammograms starting at age 40. At the same time, the authors call for increasing and ensuring equity in the availability and accessibility of mammography screenings.
- Conducting formal breast cancer risk assessments for women under 40. Women found to be at high risk would be considered for screenings and other forms of prevention before turning 40.
“Any strategy to reduce disparities statewide will take a coordinated team of community health workers, providers and other stakeholders, as well as tools and strategies to help break down barriers to care and nurture trust in health care systems. And it will require ongoing commitment,” Siegel said.
How Delaware eliminated disparities in colorectal cancer
The multi-faceted “village” model has proven successful. In 2001, the Delaware Cancer Consortium, including ChristianaCare, formed to reduce cancer rates overall.
The initiative focused closely on eliminating colorectal cancer disparities by targeting underrepresented communities most at risk of death from the disease. As a result of increasing colorectal screenings, incidences of colorectal cancer decreased by 34% for Black Delawareans, who were at greater risk of advanced disease because of lower rates of early screenings. And it reduced incidences 26% for white residents.
At the same time, colorectal cancer mortality decreased by 42% and 13% for Black and white communities, respectively, effectively eliminating a 60% higher mortality rate for Black people.
These gains have been largely sustained for more than a decade.
“We know cancer rates can be reduced when the right resources are dedicated to raising awareness of early detection and making screenings readily available and accessible,” said Nicholas Petrelli, M.D., Bank of America Endowed Medical Director of the Helen F. Graham Cancer Center & Research Institute and co-author of the commentary. Petrelli helped lead the statewide effort to eliminate the colorectal cancer disparity.
“ChristianaCare’s Office of Health Equity and a talented team of researchers, clinicians and community health experts are intentional about finding novel ways to meet communities where they are to build trust and improve health outcomes,” he said.
Equipping the village
In early October 2023, Siegel presented the plan to the Delaware Cancer Consortium’s Advisory Council and Early Detection & Prevention Committee to help garner support statewide. Such support would build on other recent breast cancer advances at ChristianaCare.
In August 2023, ChristianaCare received a $1 million grant to support the purchase of a state-of-the-art radiography system to analyze more breast cancer specimens at a faster rate. The grant will also expand a fellowship program to reduce cancer disparities, including support for this breast cancer project.
Also recently, Siegel and Jennifer Sims Mourtada, Ph.D., Christiana Care’s director of Translational Breast Cancer Research, were awarded a $309,285 grant from the National Institutes of Health to detect epigenetic risk biomarkers for TNBC. Identifying a risk biomarker will help prioritize women for earlier screening and other prevention programs to close racial disparities in breast cancer.
At the end of their commentary, the authors quote the article on eliminating colorectal cancer disparities: “’That there are complexities and nuances we do not deny, but the state of Delaware has shown us that if we have the will, there is a way.’”
They conclude: “May Delaware once again summon the will to show us the way on ending cancer disparities.”
About ChristianaCare
Headquartered in Wilmington, Delaware, ChristianaCare is one of the country’s most dynamic health care organizations, centered on improving health outcomes, making high-quality care more accessible and lowering health care costs. ChristianaCare includes an extensive network of primary care and outpatient services, home health care, urgent care centers, three hospitals (1,430 beds), a freestanding emergency department, a Level I trauma center and a Level III neonatal intensive care unit, a comprehensive stroke center and regional centers of excellence in heart and vascular care, cancer care and women’s health. It also includes the pioneering Gene Editing Institute.
ChristianaCare is nationally recognized as a great place to work, rated by Forbes as the 2nd best health system for diversity and inclusion, and the 29th best health system to work for in the United States, and by IDG Computerworld as one of the nation’s Best Places to Work in IT. ChristianaCare is rated by Healthgrades as one of America’s 50 Best Hospitals and continually ranked among the nation’s best by U.S. News & World Report, Newsweek and other national quality ratings. ChristianaCare is a nonprofit teaching health system with more than 260 residents and fellows. With its groundbreaking Center for Virtual Health and a focus on population health and value-based care, ChristianaCare is shaping the future of health care.
About the Helen F. Graham Cancer Center & Research Institute
The Helen F. Graham Cancer Center & Research Institute, a National Cancer Institute Community Oncology Research Program, is part of the ChristianaCare, one of the country’s most dynamic health systems, centered on improving health outcomes, making high-quality care more accessible and lowering health care costs. With more than 245,000 patient visits last year, the Graham Cancer Center is recognized as a national model for multidisciplinary cancer care and a top enroller in U.S. clinical research trials. In conjunction with the Gene Editing Institute, the Center for Translational Cancer Research, the Tissue Procurement Center, statewide High-Risk Family Cancer Registry and collaborations with world-renowned scientists at facilities such as The Wistar Institute in Philadelphia scientists are opening new avenues to more quickly translate cancer science into cancer medicine. For more information, visit christianacare.org/cancer.
Journal
Population Health Management
Method of Research
Commentary/editorial
Subject of Research
People
Article Title
A Population Health Proposal for Increasing Breast Cancer Screening to Reduce Racial Disparities in Breast Cancer: Getting the Village Back Together
Article Publication Date
1-Nov-2023



