In the relentless quest to combat esophageal squamous cell carcinoma (ESCC), a particularly aggressive form of cancer, recent research has shed new light on the long-term outcomes and recurrence patterns following advanced therapeutic approaches. This groundbreaking study meticulously dissects the effects of different neoadjuvant therapies in patients who have achieved pathological complete response (pCR) prior to surgery—a milestone known to correlate with improved survival rates. With emerging treatment modalities evolving rapidly, understanding how these distinct therapies influence disease recurrence and patient survival is of paramount importance for shaping future clinical strategies.
Pathological complete response signifies the absence of detectable cancer cells in surgical specimens after neoadjuvant therapy, which is treatment given before surgery to shrink tumors. While pCR is often hailed as a favorable prognostic marker in ESCC, this new comprehensive analysis delves deeper into whether the type of neoadjuvant regimen—chemotherapy alone, chemoradiotherapy, or the more novel immunochemotherapy—modulates recurrence trajectories or overall survival patterns. This approach marks a pivotal step beyond conventional survival statistics by scrutinizing how recurrences manifest subsequently, offering clues to underlying tumor biology and treatment efficacy.
In a robust retrospective cohort study encompassing 250 patients diagnosed with locally advanced ESCC, researchers classified participants into three distinct groups based on the neoadjuvant therapy received: neoadjuvant chemotherapy (NAC), neoadjuvant chemoradiotherapy (NCRT), and neoadjuvant immunochemotherapy (NICT). Each patient had successfully achieved pCR upon surgical evaluation, allowing for a focused comparison of outcomes attributable to these differing preoperative regimens. This stratification enables clinicians and scientists to assess subtleties in recurrence incidence, anatomical distribution of relapses, and long-term survival trends embedded within modern multimodal treatment landscapes.
.adsslot_ztVsYUbX7T{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_ztVsYUbX7T{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_ztVsYUbX7T{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The study’s analysis revealed a strikingly equivalent recurrence rate among the three treatment arms. Approximately 6% to 10% of patients experienced recurrence regardless of the neoadjuvant approach, a finding that challenges assumptions of superiority based solely on therapeutic modality. This equivalency suggests that while achieving pCR is a critical oncological goal, the specific preoperative treatment employed does not significantly alter the likelihood of cancer returning within the observed time frame. Such insights underscore the need for nuanced post-surgical monitoring protocols tailored more towards recurrence type than merely survival probabilities.
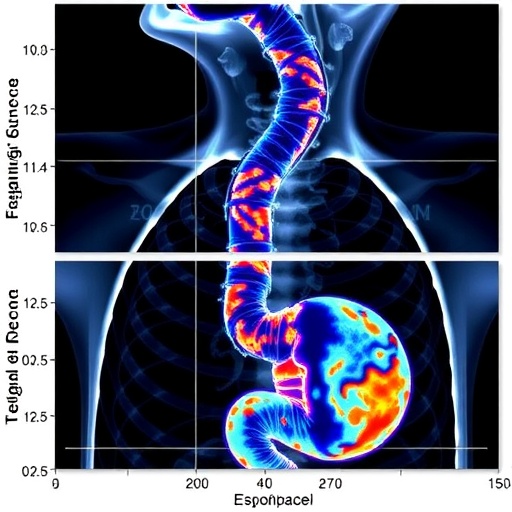
However, when dissecting the recurrence patterns themselves, notable differences emerged. Patients treated with NAC or NCRT predominantly faced distant metastatic recurrences, accounting for more than 70% of relapse cases in these cohorts. This systemic spread characterizes a more insidious form of treatment failure, whereby microscopic cancer cells evade detection and seed secondary tumors in remote organs. Conversely, the NICT group exhibited a higher prevalence of local recurrences, comprising 80% of relapses within this subset. This dichotomy highlights contrasting mechanisms of residual disease evasion and potentially differing immunological landscapes sculpted by the respective therapies.
The predominance of distant metastasis in patients receiving chemotherapy or chemoradiotherapy raises important mechanistic hypotheses. It implies that while these interventions may be effective in eradicating primary tumor sites, they might fall short in controlling disseminated microscopic cancer cells. Contrastingly, the immune-enhancing properties of immunochemotherapy could be more potent in stifling systemic spread but less capable of completely eradicating localized cancer nests, thereby increasing local recurrence risk. This complex interplay between treatment modality and tumor microenvironment warrants further molecular and immunological investigation.
Beyond recurrence, overall survival (OS) remains a crucial endpoint for patients and clinicians alike. Analyzing data over five years, the study reported 87.0% OS in the NAC group and 76.7% in the NCRT group, while the NICT cohort’s survival data was not fully evaluable due to shorter follow-up durations. Importantly, no statistically significant differences were detected in OS among the groups, reinforcing the notion that all three neoadjuvant strategies confer substantial long-term survival benefits when pCR is achieved. The absence of marked survival differences invites a broader dialogue about individualized treatment selection based on patient comorbidities, toxicity profiles, and quality of life considerations.
Event-free survival (EFS), a metric capturing survival without any signs of recurrence or progression, also showed no significant intergroup disparity. This parallelism aligns with the OS findings and strengthens confidence that pCR remains a robust prognostic biomarker irrespective of neoadjuvant regimen. Nevertheless, the numerically trending difference in EFS, favoring certain groups, suggests that larger prospective trials or meta-analyses could uncover subtle but clinically relevant distinctions presently obscured by sample size limitations.
A particularly intriguing aspect of the investigation was the differential incidence of postoperative complications, with pneumonia noted more frequently among groups—specifically with a statistically significant variation. This highlights critical perioperative considerations linked to the toxicity and immunosuppressive ramifications of the distinct therapies. Understanding how these complications interplay with long-term outcomes may guide preoperative optimization and postoperative care protocols, ultimately mitigating morbidity in this vulnerable patient population.
The variation in recurrence patterns also propels a broader immunological discourse. Immunochemotherapy’s association with predominantly local recurrences could reflect an incomplete engagement of systemic immune surveillance, or conversely, a possible suboptimal eradication of tumor cells residing within the primary anatomical domain. This insight advocates for innovative combination strategies, such as integrating immunotherapy with localized radiation or advanced surgical techniques aimed at enhancing local control, thereby potentially reducing recurrence rates further.
From a clinical perspective, these findings emphasize the indispensability of vigilant postoperative surveillance tailored to recurrence risk profiles inherent to individual neoadjuvant treatments. For patients treated with NAC or NCRT, where distant metastasis prevails, imaging surveillance protocols should prioritize systemic assessments, whereas for those receiving NICT, intensified local and regional monitoring through endoscopic and imaging modalities could facilitate early detection of recurrence amenable to salvage interventions.
Moreover, the study underscores an urgent imperative for multicenter, longitudinal research efforts. Current data, while illuminating, are confined by retrospective design and sample size constraints. Prospective trials with standardized protocols, biomarker incorporation, and extended follow-up intervals would provide heightened clarity on survival trajectories, recurrence biology, and potential predictive factors informing therapeutic decisions. Such research could catalyze the next generation of precision oncology strategies in ESCC.
In summation, the investigation marks a significant advance in esophageal cancer therapeutics by elucidating how different neoadjuvant modalities influence recurrence patterns and survival in patients reaching the coveted pCR milestone. The revelation that survival outcomes are comparable despite diverse recurrence landscapes challenges pre-existing paradigms and suggests novel pathways for post-treatment management and therapeutic innovation. It prompts clinicians to adopt nuanced, modality-specific surveillance and encourages scientists to unravel the molecular underpinnings driving these observed trends.
Ultimately, this study enriches our understanding of esophageal cancer’s complex biology in the context of cutting-edge treatments and reaffirms pathological complete response as a critical goal across all neoadjuvant regimens. As immunotherapy continues to revolutionize oncology, delineating its strengths and limitations in this setting offers a beacon of hope for optimizing patient outcomes amidst the daunting challenge of advanced esophageal cancer. Clinicians, researchers, and patients alike stand to benefit from the invaluable insights generated, which pave the way toward increasingly effective, personalized care paradigms.
Subject of Research: Recurrence patterns and long-term survival in locally advanced esophageal squamous cell carcinoma patients achieving pathological complete response after different neoadjuvant therapies followed by surgery.
Article Title: Recurrence patterns and long-term survival of locally advanced esophageal cancer patients with pathological complete response after different neoadjuvant therapies followed by surgery
Article References:
Wu, J., Qin, Y., Li, K. et al. Recurrence patterns and long-term survival of locally advanced esophageal cancer patients with pathological complete response after different neoadjuvant therapies followed by surgery. BMC Cancer 25, 1135 (2025). https://doi.org/10.1186/s12885-025-14548-4
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14548-4
Tags: advanced therapeutic approaches for ESCCCancer Treatment Strategieschemotherapy versus chemoradiotherapyesophageal cancer researchimmunochemotherapy efficacylong-term outcomes in esophageal squamous cell carcinomaneoadjuvant therapy in ESCCpathological complete response significancerecurrence patterns in esophageal cancerretrospective cohort study in oncologysurvival outcomes in cancertumor biology and treatment response