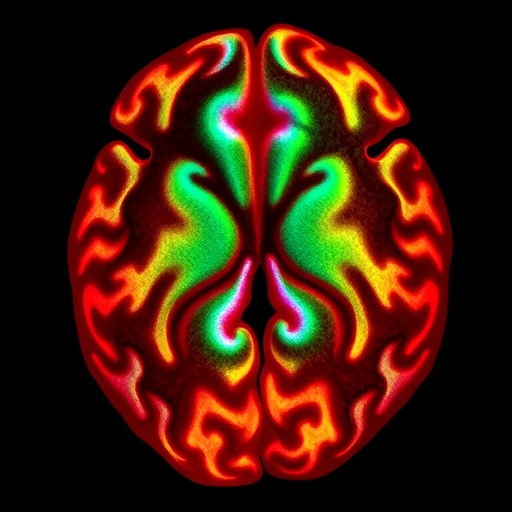
(Cambridge, Mass.) October 8, 2025 – In a groundbreaking advancement for glioblastoma research, scientists from Break Through Cancer’s Accelerating Glioblastoma Therapies Through Serial Biopsies TeamLab have demonstrated that the oncolytic virus therapy, CAN-3110, sparks a profound and previously undetectable immune response deep within recurrent glioblastoma tumors. This revelation comes from detailed molecular analyses of serial biopsies taken during a clinical trial involving two patients with recurrent glioblastoma multiforme (GBM). The findings challenge the long-held reliance on conventional imaging modalities such as MRI for evaluating therapeutic response in this aggressive brain cancer.
Glioblastoma remains one of the deadliest cancers, with dismal survival rates and limited effective treatments. Standard clinical practice has traditionally avoided repeated tissue sampling during therapy due to risks and the invasive nature of brain biopsies. Instead, oncologists have depended primarily on MRI scans to monitor tumor progression or regression. However, the new study published in Science Translational Medicine underscores the critical insights gained by coupling serial biopsies with cutting-edge multi-omics technologies. This dynamic approach has revealed intricate tumor-immune interactions and cellular shifts invisible to routine radiographic techniques.
Serial biopsies, entailing the extraction of tiny tissue samples at various time points during treatment, allowed the researchers to generate a high-resolution molecular map charting the tumor microenvironment’s evolution. The study leveraged state-of-the-art single-cell RNA sequencing, proteomics, immunopeptidomics, and AI-driven digital pathology combined with comprehensive immune cell profiling. These advanced tools uncovered a significant depletion of malignant glioma cells close to the sites of viral injection, simultaneously accompanied by a robust surge of activated immune effector cells, such as CD8+ cytotoxic and CD4+ helper T cells, mounting directed attacks against both viral and tumor-specific antigens.
Remarkably, while standard MRI scans suggested tumor enlargement—a hallmark of treatment failure—the deeper molecular investigation exposed a contrasting biological reality. The apparent volumetric increase was driven not by uncontrolled tumor growth but by immune cell infiltration and inflammation, reflecting a promising immunotherapeutic engagement. This phenomenon, sometimes referred to as pseudoprogression, complicates clinical interpretation and treatment decisions based solely on imaging surrogates.
Dr. E. Antonio Chiocca, MD, PhD, Chair of Neurosurgery at Brigham and Women’s Hospital and senior author of the study, highlights how this approach revolutionizes tumor monitoring. Instead of relying on indirect imaging indicators, serial biopsies provide a direct “real-time window” into the tumor’s molecular landscape, revealing crucial dynamics of immune response and tumor adaptation. This knowledge paves the way for more personalized and responsive treatment adjustments based on precise biological readouts rather than static imaging snapshots.
The core innovation in this trial lies in the strategic use of CAN-3110, an engineered oncolytic herpes simplex virus designed to selectively infect and lyse glioma cells while simultaneously stimulating potent anti-tumor immunity. By repeatedly administering the virus and obtaining serial tissue samples, researchers witnessed how the immune system could be effectively “trained” to recognize glioblastoma cells, even in the face of apparent radiographic progression. This discovery provides strong proof-of-concept that oncolytic virotherapy can reshape the brain tumor microenvironment to favor immune-mediated tumor eradication.
This preliminary clinical data emerged from a collaborative effort borne of Break Through Cancer’s pioneering model, uniting premier cancer research institutions including Dana-Farber Cancer Institute, Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Memorial Sloan Kettering Cancer Center, MIT’s Koch Institute for Integrative Cancer Research, and MD Anderson Cancer Center. The multidisciplinary nature of this team enabled the integration of clinical neurosurgery, molecular biology, computational pathology, and immunology techniques, highlighting the potency of collaborative science in tackling formidable cancer challenges.
The implications of these findings extend beyond glioblastoma, signaling a paradigm shift in neuro-oncology clinical trials and practice. By incorporating serial biopsies and multi-omics monitoring, future trials can better discern true therapeutic efficacy from confounding inflammatory responses, enabling earlier and more accurate treatment decisions. This refined understanding could catalyze faster development of targeted immunotherapies, ultimately improving survival outcomes in a disease where progress has been frustratingly slow.
Moreover, the study advocates for a novel biomarker-driven framework, where direct tissue interrogation complements advanced imaging to offer a composite picture of tumor biology. This approach could also facilitate identification of resistance mechanisms and adaptive changes within the tumor microenvironment, guiding combination therapies to circumvent treatment evasion.
Tyler Jacks, PhD, President of Break Through Cancer, emphasized the transformative collaboration embodied by this research. He noted that such integrative scientific endeavors are crucial to unlocking smarter, adaptive treatment strategies capable of overcoming the immunosuppressive and heterogenous nature of glioblastoma. The ability to monitor the tumor’s molecular response in near real-time represents a crucial step forward in personalized oncology.
As the clinical trial progresses with enrollment of additional patients, the research team anticipates validating these initial observations and delineating the full therapeutic potential and tolerability of CAN-3110. The well-tolerated nature of repeated biopsies observed thus far bodes well for expanding the use of this methodology, previously limited due to procedural risks.
In summary, this landmark study offers unprecedented insight into the interplay between virotherapy and immune activation within glioblastoma, challenging conventional clinical paradigms and advocating for integration of molecular multi-omics and serial biopsies in therapeutic monitoring. If broadly adopted, this approach could accelerate breakthroughs against one of the most devastating malignancies and inspire analogous strategies across oncology.
Subject of Research: People
Article Title: Serial Multi-omics Uncovers Anti-Glioblastoma Responses Not Evident by Routine Clinical Analyses
News Publication Date: 8-Oct-2025
Web References: www.breakthroughcancer.org
Keywords: Brain cancer, Clinical trials
Tags: advancements in glioblastoma researchchallenges in glioblastoma treatment monitoringclinical trials for recurrent glioblastomaglioblastoma therapy responseimmune response in glioblastomalimitations of MRI in cancer evaluationmolecular analyses of glioblastomamulti-omics technologies in oncologyoncolytic virus therapy CAN-3110real-time biopsies in cancer researchserial biopsies in brain cancertumor-immune interactions in glioblastoma