In a groundbreaking study published in the June 2025 issue of Oncotarget, researchers from multiple U.S. institutions have reported a rare cohort of pancreatic cancer patients who exhibited exceptional responses to immunotherapy. This new case series led by Kavin Sugumar and Jordan M. Winter challenges longstanding assumptions about the ineffectiveness of immunotherapy in treating pancreatic adenocarcinoma, one of the deadliest and most treatment-resistant cancers known to medicine.
Pancreatic cancer is characterized by notoriously low survival rates and a limited arsenal of effective therapeutic options. Unlike melanoma, lung cancer, and several other malignancies that have been revolutionized by immune checkpoint inhibitors, pancreatic cancer has remained largely refractory to these advances. The dense stromal microenvironment and immunosuppressive tumor milieu have collectively contributed to this resistance. However, this study isolates an intriguing subset of patients who defied this norm, demonstrating remarkable and durable responses to immune-based therapies in the absence of traditional chemotherapy regimens.
.adsslot_ONyeMA47Vi{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_ONyeMA47Vi{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_ONyeMA47Vi{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
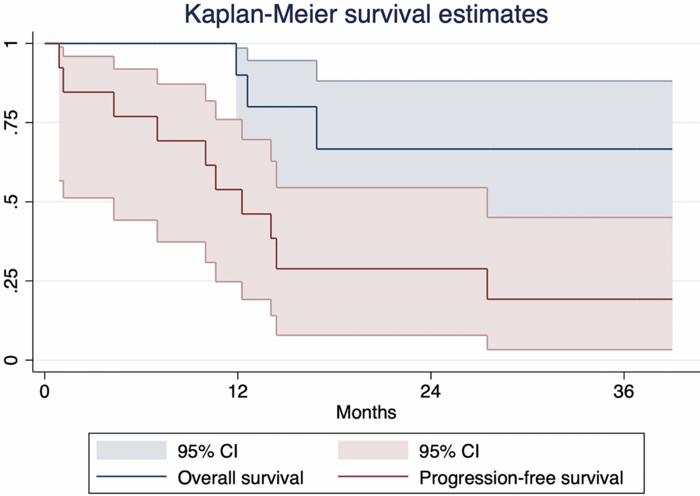
The clinical outcomes reported were unprecedented in this context. The median progression-free survival (PFS) extended to 12 months, a remarkable improvement over the typical median PFS of only a few months seen with conventional treatments in metastatic disease. Survival statistics at follow-up revealed that 80% of patients remained alive one year after treatment initiation, with a promising 70% survival rate at two years. These data paint a hopeful picture for a subset of pancreatic cancer patients who might substantially benefit from immunotherapy.
One of the most compelling observations of this study was the heterogeneity in biomarker profiles among responders. While high microsatellite instability (MSI-high) is a well-established predictive marker for immunotherapy efficacy in various cancers, especially colorectal malignancies, it was present in only a fraction of the responders in this cohort. Over half of the exceptional responders were microsatellite-stable, indicating that other, as yet unidentified, biological mechanisms may underlie their sensitivity to immunotherapy. This discovery underscores an urgent need to expand biomarker research and molecular profiling in pancreatic cancer.
The tumor microenvironment of pancreatic cancer is exquisitely complex, often characterized by a dense desmoplastic stroma rich in fibroblasts, myeloid-derived suppressor cells, and tumor-associated macrophages that collectively thwart immune infiltration and activity. The success of certain macrophage-targeting agents used in this study suggests that modulating the tumor milieu may be critical to enabling effective immune responses. This supports recent preclinical work indicating that remodeling or “re-educating” the immune microenvironment can potentiate checkpoint blockade efficacy.
This case series represents the largest to date focusing exclusively on exceptional immunotherapy responders in pancreatic cancer, marking a significant contribution to the literature. By curated selection and careful exclusion criteria, particularly removing chemotherapy confounders, the investigators provided clearer insight into the capabilities of immune modulation. The findings argue compellingly against the dogma that immunotherapy is categorically ineffective in this cancer and instead point toward a nuanced landscape where certain patients harbor biological contexts amenable to immune checkpoint inhibition.
The study’s implications extend to clinical trial design and patient selection strategies. Historically, pancreatic cancer trials have often excluded immunotherapy or included it only as an adjunct to chemotherapy, potentially obscuring its standalone potential. The current findings advocate for trials with broader inclusion criteria, incorporating detailed molecular and immunophenotypic profiling to identify and enroll patients most likely to benefit. Such precision oncology approaches could salvage immunotherapy’s promise for pancreatic cancer—not by universal application but by tailored, biomarker-driven use.
Moreover, this research highlights the limitations of current predictive biomarkers like MSI status and calls for the discovery and validation of novel predictive factors. These might include genomic signatures, tumor mutational burden beyond MSI, neoantigen landscape assessments, or immune cell infiltration patterns within the tumor microenvironment. Integrating these parameters into clinical workflows could radically reshape therapeutic paradigms.
While promising, the relatively small sample size and retrospective nature of the analysis call for cautious interpretation and compel prospective validation. Nevertheless, these compelling outcomes illuminate a path forward in a malignancy long considered nearly invulnerable to immunotherapeutic breakthroughs. Efforts to unravel the molecular and immunological underpinnings of these exceptional responses will be crucial in transforming pancreatic cancer from a grim diagnosis into a more manageable disease.
Future studies could also explore combinatorial strategies that synergize immunotherapy with novel agents targeting stromal components, metabolic pathways, or epigenetic modulators, aiming to convert immunologically “cold” tumors into “hot” ones capable of eliciting robust and durable immune attacks. The interplay between these modalities and the observed exceptional responders will further inform therapeutic innovation.
Ultimately, this study serves as a beacon of hope not only for patients but also for oncologists and researchers striving to outmaneuver one of oncology’s most formidable adversaries. It exemplifies how meticulous multi-institutional collaboration and a sharpened research focus on outliers can unveil hidden therapeutic possibilities, advocating a paradigm shift in the fight against pancreatic cancer.
Subject of Research: People
Article Title: Exceptional responders to immunotherapy in pancreatic cancer: A multi-institutional case series of a rare occurrence
News Publication Date: 10-Jun-2025
Web References:
http://dx.doi.org/10.18632/oncotarget.28739
https://www.oncotarget.com/archive/v16/
Image Credits: Copyright: © 2025 Sugumar et al. Distributed under the Creative Commons Attribution License (CC BY 4.0).
Keywords: cancer, pancreatic adenocarcinoma, immunotherapy, exceptional responders, microsatellite instability, survival
Tags: advanced pancreatic cancer case seriesdurable responses to immune-based therapiesexceptional pancreatic adenocarcinoma treatmentgroundbreaking cancer research findingsimmune checkpoint inhibitors in pancreatic cancerimmunosuppressive tumor microenvironmentinnovative treatments for metastatic cancerKavin Sugumar and Jordan M. Winter studymulti-institutional cancer researchovercoming pancreatic cancer treatment resistancePD-1 and CTLA-4 blockade therapiesrare pancreatic cancer immunotherapy response