Drug may break up ‘neutrophil extracellular traps,’ or NETs, which contribute to lung inflammation and thicken mucus
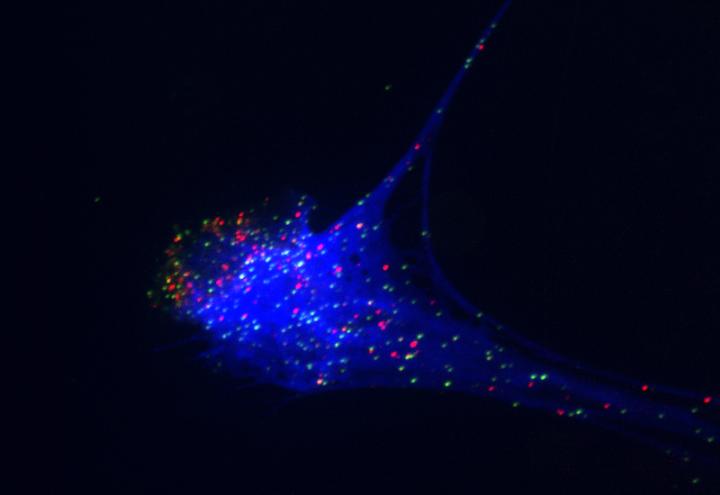
Credit: Lucas de Meglio and Patrick Munzer, Boston Children’s Hospital
BOSTON — Researchers at Boston Children’s Hospital and Brigham and Women’s Hospital have launched a randomized, placebo-controlled clinical trial of dornase alfa (Pulmozyme) in patients with severe COVID-19 pneumonia and respiratory failure requiring mechanical ventilation. The study aims to enroll 60 adults and children (over age 3) admitted to intensive care units.
Dornase alfa, also called DNase 1, is FDA-approved for patients with cystic fibrosis, to break up thick mucus secretions and prevent lung infections. The trial is supported by the Massachusetts Consortium on Pathogen Readiness, and the drug is being provided by Genentech, a member of the Roche Group, which is also providing supplementary financial support.
“We hope this drug, which is known to be safe, will help reduce the inflammation that contributes to worsening respiratory distress in COVID-19,” says Benjamin Raby, MD, MPH, chief of the Division of Pulmonary Medicine at Boston Children’s Hospital and principal investigator on the study.
The 18-month study will randomize patients to twice-daily nebulized dornase alfa or placebo (a saline solution) within 48 hours after intubation and placement on a ventilator. Treatments will be given via the ventilator tubing, twice a day for up to 28 days. Researchers will then monitor both groups for up to 28 days, or until patients are no longer receiving mechanical ventilation, whichever is sooner. Neither the researchers nor the patients (and families) will know which treatment is being given.
The main outcome of interest is the number of patients in each group who are alive and ventilator-free 28 days after treatment. Other measures will include airway resistance to breathing, lung compliance (the lungs’ ability to stretch and expand), blood oxygenation, and length of stay in the ICU and hospital.
Why dornase alfa for COVID-19 pneumonia?
Some patients with COVID-19 pneumonia produce large amounts of thick mucus that can make effective delivery of oxygen by mechanical ventilation more challenging. Dornase alfa is an effective mucolytic — able to soften mucus and promote its clearance from the airways. In addition, dornase alfa may be able to reduce lung inflammation promoted by neutrophil extracellular traps, or NETs. NETs are webs of DNA and toxic protein released by neutrophils, first responders in the immune system, in an excessive effort to entrap invading microbes. NETs are also known to produce dangerous blood clots such as those that form in COVID-19 patients, and are known, in general, to contribute to blood clots in the lung capillaries, inflammation, and lung injury.
Denisa Wagner, PhD, of the Program in Cellular and Molecular Medicine at Boston Children’s Hospital, who helped to initiate the new trial, has been studying NETs and their role in unwanted clot formation and fibrosis (thickening and scarring of tissue) for more than a decade.
“Preclinical studies by several groups, including ours at Boston Children’s Hospital, have found that DNase 1 improved outcome in lung injury models and thrombotic models mimicking events that occur frequently in COVID-19, such as deep vein thrombosis, stroke and microvascular thrombosis,” Wagner says. “This suggests to us that treatment with DNase could be beneficial in severe lung injury observed in COVID-19.”
Although this study is limited to the lung, it’s hypothesized that NETs contribute to coagulopathies seen with COVID-19 elsewhere in the body.
###
Other study principals include Rebecca Baron, MD, and Laura Fredenburgh, MD, of Brigham and Women’s Hospital and Meera Subramaniam, MD, and Gregory Sawicki, MD, of Boston Children’s Hospital.
Boston Children’s Hospital is ranked the #1 children’s hospital in the nation by U.S. News & World Report and is the primary pediatric teaching affiliate of Harvard Medical School. Home to the world’s largest research enterprise based at a pediatric medical center, its discoveries have benefited both children and adults since 1869. Today, 3,000 researchers and scientific staff, including 9 members of the National Academy of Sciences, 21 members of the National Academy of Medicine and 12 Howard Hughes Medical Investigators comprise Boston Children’s research community. Founded as a 20-bed hospital for children, Boston Children’s is now a 415-bed comprehensive center for pediatric and adolescent health care. For more, visit our Discoveries blog and follow us on social media @BostonChildrens, @BCH_Innovation, Facebook and YouTube.
Media Contact
Erin Tornatore
[email protected]




