A groundbreaking clinical investigation has revealed a transformative approach in the management of recurrent prostate cancer presenting with limited metastatic spread, known as oligometastatic disease. This pioneering Phase II trial, dubbed LUNAR, explored the efficacy of combining a radiopharmaceutical agent with stereotactic body radiation therapy (SBRT) compared to SBRT alone. The results signify a significant leap forward, demonstrating markedly prolonged progression-free survival in patients receiving the novel combination, heralding a new frontier in personalized cancer therapy.
Prostate cancer, when recurrent and metastatic, poses substantial therapeutic challenges, particularly when cancer cells colonize only a few distinct sites distant from the primary tumor. In the oligometastatic state, characterized by up to five metastatic lesions, high-precision radiation modalities like SBRT have become increasingly prevalent. SBRT permits the administration of ablation-dose radiation with pinpoint accuracy, targeting tumors while sparing healthy tissue. However, microscopic disease that eludes even state-of-the-art imaging has remained a critical barrier, often precipitating relapse despite local control.
The LUNAR trial’s innovation lies in synergistically combining SBRT with a radiopharmaceutical agent, ^177Lu-PNT2002, which homes in on prostate-specific membrane antigen (PSMA) expressed abundantly on prostate cancer cells. This radioligand therapy delivers targeted beta particle emissions directly to cancer cells throughout the body, addressing both visible and occult metastases. Until now, such radiopharmaceuticals were mainly deployed in advanced, late-stage disease. LUNAR investigated their potential as a neoadjuvant treatment in earlier metastatic phases, in conjunction with precise metastasis-directed radiation.
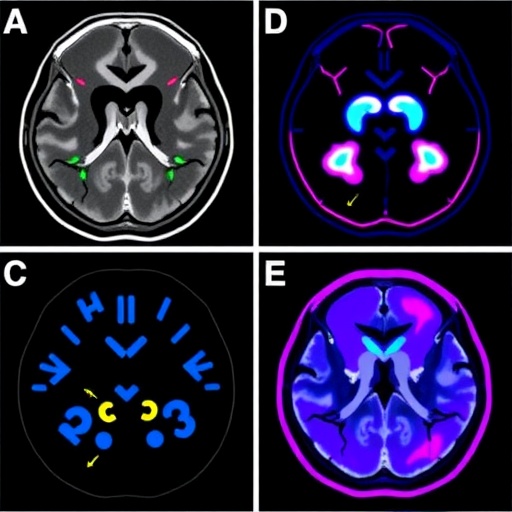
Ninety-two men with hormone-sensitive oligometastatic prostate cancer were randomly allocated to receive either SBRT alone or the investigational radiopharmaceutical followed by SBRT. Patients had one to five metastatic lesions confirmed via PSMA PET/CT, an imaging modality delivering unprecedented sensitivity and tumor detection accuracy. Follow-up involved meticulous biochemical (PSA level) monitoring and scheduled imaging to assess disease progression.
Remarkably, patients receiving the combination of ^177Lu-PNT2002 and SBRT exhibited a median progression-free survival of 18 months, more than doubling the seven months observed in the SBRT-only cohort. The statistical significance (p<0.001) reinforces the robust efficacy of this integrated approach. The enhanced therapeutic impact endured even after controlling for baseline PSA, hormonal therapy history, and lesion count, underscoring the radiopharmaceutical’s role as an independent contributor to improved outcomes.
A profoundly consequential finding was the substantial delay in initiation of androgen deprivation therapy (ADT) among patients treated with the combination regimen. ADT, while standard in recurrent prostate cancer, is associated with debilitating side effects including fatigue, osteoporosis, metabolic disturbances, and cardiovascular risks. Patients on the novel therapy deferred ADT for an average of 24 months, compared to 14 months for those receiving radiation alone, potentially translating to enhanced quality of life and reduced treatment-related morbidity.
Assessment of PSA responses further elucidated therapeutic benefits; 52% of patients in the combination arm achieved a PSA reduction of 50% or greater, compared to 31% in the SBRT-only group. Such biochemical responses portend durable clinical benefits and reinforce the synergy achieved by integrating systemic radiopharmaceutical therapy with localized radiation.
Crucially, the local control rates attained through SBRT were extraordinarily high—98% for radiation alone and a perfect 100% with the addition of ^177Lu-PNT2002—indicating undercurrent microscopic disease driving progression rather than failure at previously treated sites. Indeed, 98% of progression events represented new metastatic growths, highlighting the critical need for systemic treatment strategies to complement radiation.
Safety profiles between treatment arms were comparable, with no significant increase in severe adverse events seen upon addition of the radiopharmaceutical. Grade 3 toxicities were largely confined to transient leukopenia, affecting only a small minority of patients across both arms. This favorable tolerability underscores the clinical feasibility of employing radioligand therapy in earlier disease stages without incurring prohibitive toxicity.
The LUNAR trial thus positions ^177Lu-PNT2002-mediated radiopharmaceutical therapy as a promising adjunct to definitive radiation in oligometastatic prostate cancer, delivering a dual assault on both apparent and occult disease compartments. This approach could redefine standards of care, shifting paradigms from sequential therapies to integrated multimodal regimens that maximize disease control while preserving patient well-being.
Notably, prior investigations employing radiopharmaceuticals targeting bone metastases exclusively have not demonstrated similar benefits, emphasizing the importance of PSMA-targeting agents that directly engage tumor cells irrespective of location. This nuanced understanding differentiates LUNAR’s approach and offers plausible mechanistic insights into improved outcomes.
Despite these advances, the challenge of residual microscopic disease remains unresolved, as 64% of combination therapy recipients eventually experienced progression. This limitation highlights the necessity for continued research refining dosing strategies, treatment sequencing, and developing next-generation agents with enhanced tumor selectivity and radiobiologic potency.
Currently, ^177Lu-PNT2002 remains investigational for oligometastatic recurrent prostate cancer, accessible only within clinical trials. However, both SBRT and PSMA PET/CT are FDA-approved and increasingly integrated in clinical practice, paving a practical path toward wider adoption of combined modality therapies pending regulatory approvals and further validation.
In conclusion, the LUNAR study heralds a paradigm shift in treating oligometastatic prostate cancer by demonstrating that neoadjuvant PSMA-targeted radiopharmaceuticals significantly enhance radiation efficacy, prolong progression-free survival, and meaningfully delay systemic hormonal therapy. As mechanistic insights deepen and clinical protocols refine, this integrated therapeutic avenue holds great promise to improve patient outcomes in a disease historically marked by complex recurrence dynamics.
Subject of Research:
Oligometastatic recurrent prostate cancer; radiopharmaceutical and radiation therapy combination
Article Title:
Novel Radiopharmaceutical Plus Radiation Therapy Significantly Extends Progression-Free Survival in Oligometastatic Prostate Cancer: Insights from the Phase II LUNAR Trial
News Publication Date:
September 28, 2025
Web References:
ASTRO Annual Meeting 2025
LUNAR Abstract
Related ASCO Publication
References:
Data and results presented at the American Society for Radiation Oncology (ASTRO) 2025 Annual Meeting, reported by Dr. Amar U. Kishan and colleagues.
Keywords:
Prostate cancer, oligometastatic disease, radiopharmaceutical therapy, ^177Lu-PNT2002, PSMA-targeted therapy, stereotactic body radiation therapy (SBRT), progression-free survival, androgen deprivation therapy, metastasis-directed therapy, clinical trial, precision oncology