Imaging findings of in situ pulmonary artery thrombosis associated with radiation therapy are different from acute pulmonary emboli and do not appear to embolize
Credit: American Roentgen Ray Society (ARRS), American Journal of Roentgenology (AJR)
Leesburg, VA, October 9, 2020–According to an article in ARRS’ American Journal of Roentgenology (AJR), the imaging findings of in situ pulmonary artery thrombosis (PAT) associated with radiation therapy (RT) are different from those of acute pulmonary emboli and do not appear to embolize. Due to the differences in clinical prognosis and subsequent management strategies, in situ PAT associated with RT–“which to our knowledge has not previously been described in the English literature,” wrote the authors of this AJR article–must be distinguished from pulmonary embolism.
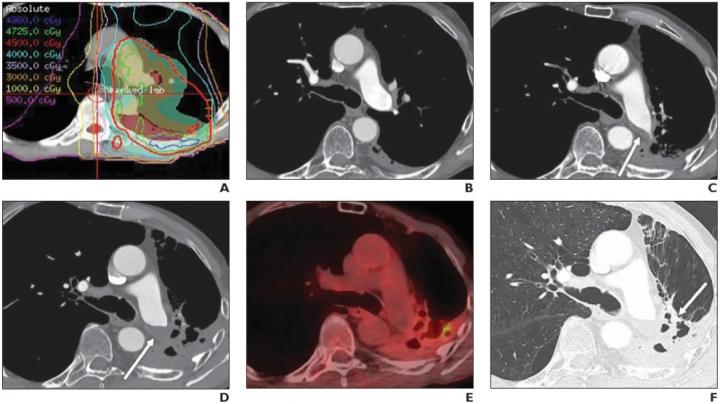
Searching the radiology database of a large teaching hospital to identify patients who had PAT develop after receiving RT, first author Jitesh Ahuja from the thoracic imaging department at the University of Texas’ MD Anderson Cancer Center recorded the PAT’s CT characteristics: number, location, appearance of filling defects, as well as the presence of associated lung fibrosis. The terminology (in situ thrombosis vs acute or chronic pulmonary embolism) used to describe PAT, the time between completion of RT and development of PAT, the size change of PAT, and any observation of new thrombi and emboli on follow-up imaging were also recorded.
With a study population consisting of 27 patients (19 men and eight women) at a mean age of 71 (range, 54-90 years), the primary malignancy was lung cancer in 22 patients (81%) and mesothelioma in five patients (19%). Whereas most PATs were solitary (93%) and nonocclusive (96%) and formed an obtuse angle to the vessel wall (89%), all PATs were eccentric within the involved pulmonary artery and located within the RT volume. The time from completion of RT to initial diagnosis of PAT on CT ranged from 53 to 2,522 days (mean, 675 days). In all patients, CT findings of radiation-induced lung fibrosis were present in the lung supplied by the affected pulmonary artery. “On follow-up imaging, none of the patients were observed to have filling defects develop in other parts of the PA, which would have suggested embolization,” Ahuja et al. added.
Acknowledging that RT is a “key choice” in multimodality treatment of intrathoracic malignancies, the authors noted that RT-associated cardiovascular complications remain the leading non-cancer-related cause of morbidity and mortality among cancer survivors. “Radiologist awareness of PAT can facilitate accurate diagnosis and impact management,” they concluded.
###
Founded in 1900, the American Roentgen Ray Society (ARRS) is the first and oldest radiological society in North America, dedicated to the advancement of medicine through the profession of radiology and its allied sciences. An international forum for progress in medical imaging since the discovery of the x-ray, ARRS maintains its mission of improving health through a community committed to advancing knowledge and skills with an annual scientific meeting, monthly publication of the peer-reviewed American Journal of Roentgenology (AJR), quarterly issues of InPractice magazine, AJR Live Webinars and Podcasts, topical symposia, print and online educational materials, as well as awarding scholarships via The Roentgen Fund®.
Media Contact
Logan K. Young
[email protected]
Related Journal Article
http://dx.




