Pancreatic cancer has long been recognized as one of the deadliest malignancies, notorious for its late diagnosis, aggressive progression, and limited therapeutic options. Despite substantial advances in oncology, the promise of immunotherapy—a breakthrough in numerous other cancer types—has historically fallen short in the context of pancreatic neoplasms. However, a pioneering study spearheaded by investigators at UCLA represents a significant stride towards bridging this gap. Their work evaluates the safety and potential efficacy of integrating immunotherapy with standard chemotherapy prior to surgery in patients with borderline-resectable pancreatic cancer, a stage where surgical removal is challenging yet still feasible.
The study is distinctive primarily because it targets borderline-resectable pancreatic cancer, a clinical categorization characterized by tumor localization that invites surgical intervention but is complicated by vascular involvement or other anatomical challenges. The integration of immunotherapy with the chemotherapy regimen known as modified FOLFIRINOX, which consists of fluorouracil, leucovorin, irinotecan, and oxaliplatin, was tested to investigate whether this combination could improve both the likelihood of successful surgical resection and overall patient outcomes. The immunotherapeutic agent employed was nivolumab, an immune checkpoint inhibitor targeting the PD-1 receptor, known for its role in reinvigorating exhausted T cells in other malignancies.
Conducted as a single-arm Phase 1b/2 clinical trial, this study enrolled 28 patients, thus creating an opportunity to gather real-world data on treatment responses in a nuanced patient population. By administering combined therapy in the neoadjuvant (preoperative) setting, researchers gained the unique advantage of obtaining tumor tissue from surgical specimens for comprehensive analyses. These analyses included high-resolution techniques such as gene expression profiling, immunohistochemistry, and spatial transcriptomics, enabling a multidimensional understanding of the tumor immunobiology and how it evolves following this treatment regimen.
Remarkably, the combination therapy was well tolerated, with patients experiencing limited immune-related adverse events and no delays impacting the timing of surgery. This is especially notable given the complexity of integrating immunotherapy with intensive chemotherapy, both of which have significant toxicities. Among the patients, 79% proceeded to surgery, and all who underwent resection achieved complete tumor removal. Surgical margins were negative in the vast majority (86%), and half of these patients displayed no detectable cancer within their lymph nodes at the time of surgery, a factor indicative of successful tumor burden reduction.
Although the overall survival rates in this cohort did not significantly surpass historical controls treated with chemotherapy alone, the study illuminated that a distinct subset of patients experienced profound and sustained tumor regression. Approximately 9% demonstrated a complete pathological response, meaning no residual cancer cells were found upon surgical examination, while another 9% exhibited near-complete responses. These findings suggest that while the addition of immunotherapy may not broadly enhance survival outcomes, it substantially benefits certain individuals, pointing towards an underlying heterogeneity in tumor-immune interactions within this patient population.
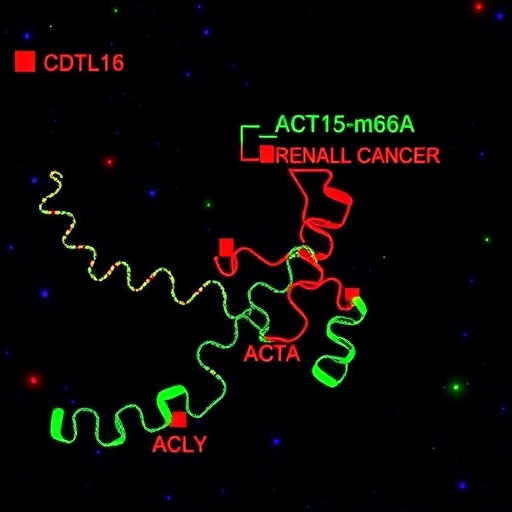
The integrated immune profiling revealed that the introduction of nivolumab alongside chemotherapy significantly boosted immune activation within the tumor microenvironment. This was evidenced by elevated infiltration of CD8+ cytotoxic T lymphocytes, cells fundamentally responsible for recognizing and eradicating malignant cells. Contrastingly, the treatment also appeared to induce disorganization within immune cell clusters and fostered an accumulation of plasma cells and exhausted T cells. Exhausted T cells, characterized by diminished effector function despite antigen recognition, likely represent an immune escape mechanism employed by pancreatic tumors to circumvent immune-mediated destruction, thus explaining the limited success of immunotherapy in many cases.
These insights are vital, shedding light on the dualistic nature of immunotherapy’s impact on tumor immunity in pancreatic cancer. While immune activation is essential for therapeutic efficacy, concurrent immune disarray and exhaustion can undermine the potential for long-lasting tumor control. Understanding these mechanisms provides a roadmap for future therapeutic strategies, emphasizing the need for treatments that not only stimulate immune responses but also preserve or restore immune organization and function within the tumor microenvironment.
This research carries profound implications for pancreatic cancer treatment paradigms. It underscores that while immunotherapy combined with chemotherapy is safe and shows promise in enhancing resectability and inducing dramatic tumor regressions in a subset of patients, it is not a universal solution. Instead, it propels the field towards more personalized approaches that may include biomarkers for patient selection and adjunct therapies to overcome immune exhaustion. By advancing these avenues, clinicians hope to transform immunotherapy from a limited niche treatment into a cornerstone of pancreatic cancer management.
The study team was multidisciplinary, combining expertise in surgical oncology, immunology, and translational research. Led by Dr. Timothy Donahue, chief of surgical oncology and a professor at the David Geffen School of Medicine at UCLA, the investigators leveraged the resources of the UCLA Health Jonsson Comprehensive Cancer Center and the Agi Hirshberg Center for Pancreatic Diseases. The collaboration allowed the establishment of a robust platform for evaluating novel therapeutic combinations with a translational research focus, linking clinical outcomes to molecular and immunological correlates derived from patient specimens.
Future research directions inspired by this study include efforts to delineate the molecular and immunological characteristics that predict robust responses to combined immunotherapy and chemotherapy. Additionally, refining treatment schedules and exploring combination regimens that target immune exhaustion pathways—such as co-inhibitory receptors beyond PD-1 or interventions modulating plasma cell activity—may enhance the depth and durability of responses. The ability to perform head-to-head comparisons between pretreatment biopsies and surgical tumor specimens is a powerful tool that will continue to inform adaptive clinical trial designs.
In summary, the UCLA investigators have initiated a pivotal exploration into the use of immunotherapy in a pancreatic cancer subgroup that is difficult to treat but potentially curable with surgery. Their findings highlight both the potential and the challenges of this approach, indicating that while a substantial portion of patients may not derive a clear survival benefit, a meaningful minority experience remarkable disease regression. This nuanced understanding of pancreatic tumor immunobiology lends hope for more effective treatments and better outcomes for a malignancy that has traditionally been refractory to immunotherapeutic strategies.
By melding precise clinical intervention with cutting-edge immunological investigation, the study exemplifies the modern oncology research ethos: combining patient-centered therapeutic innovation with deep biological inquiry. Such integrative efforts are essential to unraveling the complexities of pancreatic cancer and to ultimately altering its grim prognosis. The work of Dr. Donahue, Dr. Wainberg, Dr. Link, and their colleagues thus sets a new benchmark for how immunotherapy can be rationally employed and optimally timed to benefit patients harboring this devastating disease.
Subject of Research:
Borderline-resectable pancreatic cancer treatment using combined immunotherapy (nivolumab) and chemotherapy (modified FOLFIRINOX) in the neoadjuvant setting.
Article Title:
Not explicitly stated; the study findings published in Nature Communications focus on immunotherapy added to chemotherapy before surgery in borderline-resectable pancreatic cancer.
News Publication Date:
Not explicitly stated in the text.
Web References:
– UCLA Health Jonsson Comprehensive Cancer Center: https://www.uclahealth.org/cancer
– Full article DOI: https://doi.org/10.1038/s41467-026-68976-2
References:
Donahue, T., Wainberg, Z., Link, J. et al. (2024). [Title as per article in Nature Communications]. Nature Communications. DOI: 10.1038/s41467-026-68976-2.
Image Credits:
No specific image credit provided.
Keywords:
Pancreatic cancer, cancer immunotherapy, immunotherapy, chemotherapy, modified FOLFIRINOX, nivolumab, borderline-resectable pancreatic cancer, tumor microenvironment, immune exhaustion, CD8 T cells, translational research, neoadjuvant therapy.
Tags: borderline-resectable pancreatic cancer treatmentclinical trials for pancreatic cancer treatmentcombination therapy in pancreatic neoplasmsefficacy of immunotherapy in pancreatic cancermodified FOLFIRINOX chemotherapy regimennivolumab immune checkpoint inhibitorovercoming challenges in pancreatic tumor resectionPD-1 receptor targeting in cancer therapypreoperative immunotherapy and chemotherapy for pancreatic cancerreinvigorating T cells in cancer immunotherapysafety of immunotherapy with chemotherapysurgical outcomes after neoadjuvant therapy