Emerging research is shedding new light on the prognosis of melanoma, specifically focusing on the risk of recurrence in patients who have undergone surgery for stage I-III melanoma. Despite advances in adjuvant therapies, predicting which patients are most likely to experience relapse remains a clinical challenge. A recent study published in BMC Cancer explores the potential of circulating tumor DNA (ctDNA) along with genomic and clinical factors to forecast disease-free survival and recurrence risk more accurately.
Melanoma, a notoriously aggressive skin cancer, has seen improvements in treatment, especially with the advent of immunotherapies such as anti-PD-1 agents. While these therapies offer hope, not all patients benefit equally, underscoring the importance of effective biomarkers to stratify patients by risk. The study conducted targeted next-generation sequencing (NGS) on tumor samples from 55 melanoma patients across stages I to III and analyzed postsurgical plasma samples from 46 of these individuals to detect ctDNA mutations.
The investigation utilized a comprehensive panel encompassing 437 cancer-related genes, enabling a robust genomic profiling of primary tumors. This approach allowed researchers to examine not only common driver mutations like BRAF, NRAS, and KIT but also more complex genomic alterations that might influence patient outcomes. The study’s median disease-free survival (DFS) reached approximately 39.2 months, illustrating the variability in patient prognoses following surgical intervention.
One pivotal finding was the observed enhancement in DFS among patients receiving anti-PD-1 adjuvant therapy compared to those treated with interferon. The median DFS was not reached in the former group, whereas it was 21.3 months for the latter, demonstrating a statistically significant benefit of immunotherapy. However, strikingly, the presence of canonical driver mutations such as BRAF, NRAS, and KIT did not correlate significantly with DFS, challenging the conventional emphasis placed upon these alterations in prognostic assessments.
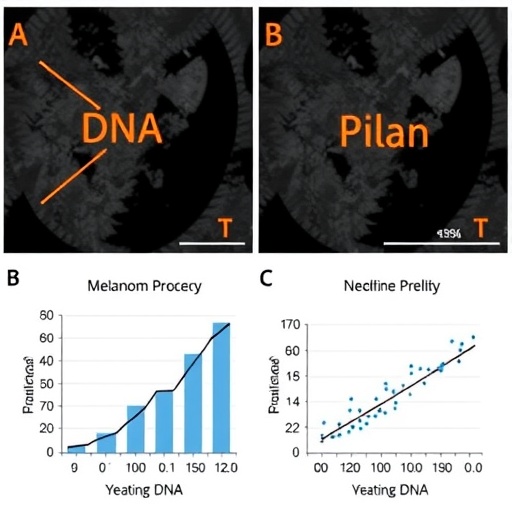
In contrast, chromosomal instability score (CIS) emerged as a robust independent predictor of disease-free survival. Patients with a high CIS exhibited considerably worse outcomes, with a median DFS of 14.3 months versus 49.7 months for those with low CIS. This finding highlights chromosomal instability as an overarching genomic feature that may reflect tumor aggressiveness and propensity for relapse, transcending the predictive value of single-gene mutations.
The study further incorporated analysis of circulating tumor DNA in postsurgical plasma. CtDNA represents tumor-derived fragmented DNA freely circulating in the bloodstream and is increasingly recognized as a dynamic biomarker that mirrors tumor burden in real time. A maximum variant allele frequency (maxVAF) exceeding 1% in ctDNA after surgery was strongly associated with poorer DFS, emphasizing its utility for early detection of minimal residual disease and impending recurrence.
Integrating CIS and postsurgical ctDNA status provided a powerful combinatorial framework for recurrence risk prediction. Not only do these markers independently forecast outcomes, but their combined assessment may refine patient stratification, guiding surveillance intensity and adjuvant treatment decisions. The implications for personalized medicine are profound, as clinicians could tailor therapeutic strategies based on molecular and circulating biomarkers rather than relying solely on clinical staging.
This work underscores a paradigm shift, spotlighting the genomic architecture of melanoma and ctDNA as critical tools in the ongoing battle against metastatic progression. The identification of high-risk patients immediately after surgery could enable timely intervention, possibly altering the natural history of the disease. Moreover, continuous monitoring of ctDNA might facilitate early therapeutic alterations in patients poised for relapse, enhancing efficacy and survival rates.
Technical advances in next-generation sequencing have made it feasible to perform expansive genomic assessments on tumor tissue and plasma samples, providing a multidimensional view of disease biology. This comprehensive approach reveals the heterogeneity inherent in melanoma and the complex interplay of genetic and genomic instability factors driving recurrence. It also exemplifies the potential of liquid biopsies to revolutionize oncology by offering minimally invasive, real-time insights.
While driver gene mutations have dominated oncologic diagnostics for years, this study illustrates the limitations of focusing solely on these alterations. Instead, chromosomal instability and the dynamic presence of ctDNA reflect global tumor behavior more effectively, offering a holistic snapshot of tumor biology. Future therapeutic protocols may incorporate these biomarkers to optimize adjuvant therapy allocation, sparing low-risk patients from unnecessary toxicity and intensifying treatment in those with elevated relapse risk.
Importantly, the study paves the way for ongoing research to validate these findings in larger, more diverse cohorts. The challenge remains to standardize CIS and ctDNA quantification methods and integrate them into clinical workflows. Nonetheless, the promising prognostic capabilities highlighted underscore the potential of these markers to transform melanoma management fundamentally.
In summary, the identification and validation of chromosomal instability scores alongside circulating tumor DNA levels provide a powerful prognostic toolkit for early detection of melanoma recurrence. These findings promise to enhance clinical decision-making by merging molecular diagnostics with traditional staging, ushering in more precise, personalized melanoma care.
The continued evolution of genomic technologies and liquid biopsy assays will undoubtedly refine risk prediction algorithms, enabling clinicians to intervene earlier and more effectively. This fusion of genomic instability metrics and ctDNA profiling heralds a new era in melanoma treatment strategies aimed at improving patient outcomes and survival in this challenging malignancy.
Subject of Research: Recurrence risk prediction in resected stage I-III melanoma using circulating tumor DNA and genomic biomarkers.
Article Title: Recurrence risk prediction in resected stage I-III melanoma utilizing circulating tumor DNA
Article References:
Zhao, M., Zhao, L., Yang, Y. et al. Recurrence risk prediction in resected stage I-III melanoma utilizing circulating tumor DNA. BMC Cancer 25, 1808 (2025). https://doi.org/10.1186/s12885-025-15093-w
Image Credits: Scienmag.com
DOI: 10.1186/s12885-025-15093-w
Tags: adjuvant therapies for melanomabiomarkers for melanoma risk stratificationcancer-related gene panel studiescirculating tumor DNA analysisclinical factors influencing melanoma outcomesctDNA mutations in melanomadisease-free survival in cancer patientsgenomic profiling in melanomaimmunotherapy response in melanoma patientsmelanoma recurrence predictionstage I-III melanoma prognosistargeted next-generation sequencing in oncology