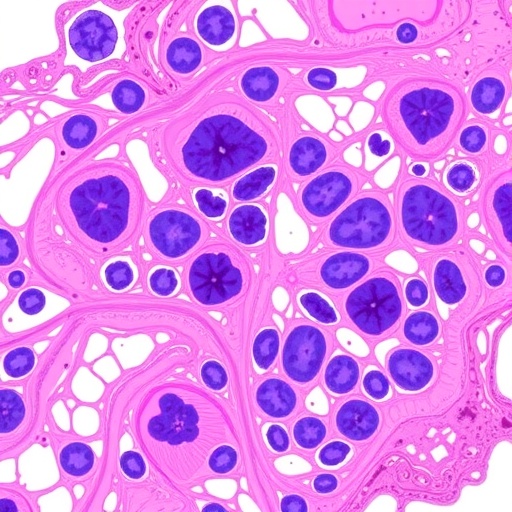
In an unprecedented retrospective study encompassing over 11,000 patients, researchers at West China Second University Hospital (WCSUH) have shed new light on the often elusive risk factors behind undetected cervical cancer in women initially diagnosed with high-grade cervical intraepithelial neoplasia (CIN). This comprehensive investigation, published in the renowned journal BMC Cancer, delves deeply into the nuanced predictive value of combining cytology with endocervical curettage (ECC) — a diagnostic confluence with promising clinical implications for early cancer detection.
For decades, cervical cancer screening has relied heavily on cytological evaluations and human papillomavirus (HPV) testing. However, even in the presence of high-grade precancerous lesions identified by biopsy, a subset of patients harbor undiagnosed invasive cancers that escape initial detection. These “hidden” malignancies pose a significant clinical challenge, often resulting in delayed diagnosis and compromised patient outcomes. The WCSUH team’s study aimed to identify robust clinical and pathological predictors that might effectively signal the presence of these undetected cancers.
The study cohort consisted of 11,651 women with biopsy-confirmed high-grade CIN, observed over five years. Following surgical treatment, 229 patients were ultimately diagnosed with invasive cervical cancer, revealing the critical clinical problem of lesions that disguise their true malignant potential. Leveraging multivariate logistic regression, the investigators identified a constellation of independent risk factors that markedly elevated the probability of undetected cancer at the time of initial biopsy.
.adsslot_1o3DXvqbac{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_1o3DXvqbac{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_1o3DXvqbac{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Among the most significant contributors was advancing age. The statistical model quantified this risk with an odds ratio (OR) of 1.10 per year, underscoring that older patients are increasingly vulnerable to harboring invasive disease beneath their high-grade CIN diagnosis. This finding reinforces the need for heightened clinical vigilance in older women presenting with cervical lesions.
Equally noteworthy was the symptomatology of abnormal vaginal bleeding. Women presenting with this clinical sign demonstrated nearly a threefold increase in the risk (OR = 2.94) for underlying invasive carcinoma. This harbinger symptom could potentially serve as an accessible clinical flag, triggering more aggressive diagnostic scrutiny when detected in conjunction with high-grade CIN.
The study further elucidated the pivotal role of HPV infection subtypes. Infection with HPV16 or HPV18, the oncogenic strains most strongly linked to cervical carcinogenesis, independently predicted a 2.56-fold increase in cancer risk. Interestingly, infection with a single HPV type was also shown to confer a higher risk compared to multiple-type infections, challenging previous assumptions and suggesting that viral clonality might influence disease trajectory.
Turning to cytological assessments, the presence of atypical squamous cells, cannot exclude HSIL (ASC-H), emerged as a formidable predictor with an odds ratio of 3.77. Similarly, cytology revealing high-grade squamous intraepithelial lesions (HSIL) portended even greater risk (OR = 4.65), emphasizing the critical importance of detailed cytological interpretation when triaging patients for further intervention.
Another pathological hallmark identified was endocervical glandular involvement. This subtle but significant finding conferred a modest yet statistically significant risk increase (OR = 1.59), highlighting the necessity of thorough endocervical sampling during diagnostic evaluation to avoid underestimating disease extent.
The crux of the study centers on the innovative Cytology-ECC index, a composite scoring system developed by integrating cytological data with results from endocervical curettage. This combined index demonstrated superior predictive accuracy with an area under the receiver operating characteristic curve (AUC) of 0.787, surpassing the diagnostic performance of cytology or ECC alone. Such an advancement offers a compelling tool for clinicians, potentially enabling more precise stratification of patients at risk for invasive disease.
This enhanced predictive capability holds transformative implications for clinical decision-making. By integrating multifactorial risk determinants into a unified model, healthcare providers might better identify patients who require expedited surgical management or more rigorous surveillance, thereby reducing the incidence of delayed cervical cancer diagnoses.
The significance of these findings resonates beyond the immediate clinical environment. In resource-limited settings where advanced imaging and molecular diagnostics may be inaccessible, the Cytology-ECC index offers a cost-effective and pragmatic framework grounded in established testing modalities, promising wider global applicability.
Moreover, this comprehensive study highlights the interplay between viral oncogenesis, host factors, and histopathological findings in dictating patient outcomes. By elucidating independent risk factors and harnessing their combined predictive power, the investigation paves the way for personalized risk assessment paradigms in cervical cancer screening programs.
Looking forward, these results advocate for increased adoption of integrated diagnostic approaches in gynecological oncology. Further prospective validation studies across diverse populations will be instrumental in refining the Cytology-ECC index, optimizing cutoffs, and embedding this methodology into standardized screening algorithms.
In parallel, the identification of specific demographic and clinical predictors enhances our understanding of cervical carcinogenesis, informing targeted patient counseling and follow-up strategies. For instance, older women presenting with abnormal bleeding and high-grade cytology findings in the context of HPV16/18 infection may benefit from prioritized surgical evaluation.
The clinical utility of endocervical glandular involvement as a subtle marker of invasive potential stresses the importance of comprehensive lesion mapping during biopsy, advocating for meticulous pathological assessment protocols to ensure no areas of concern are overlooked.
Taken together, the breakthrough insights from this expansive cohort study invigorate efforts to reduce cervical cancer morbidity by addressing diagnostic blind spots in high-grade CIN patients. They underscore a paradigm shift towards multidimensional risk evaluation, wherein combining cytology with ECC findings yields a more nuanced and actionable clinical picture.
This research not only advances scientific understanding but also sparks hope for improved patient outcomes through earlier, more accurate detection of invasive disease in populations at risk. The strategic application of the Cytology-ECC index in clinical practice holds promise for transforming cervical cancer management globally, emphasizing prevention and early intervention.
As cervical cancer continues to remain a leading cause of cancer-related mortality among women worldwide, innovations such as this offer a beacon of progress. They illuminate pathways to closing diagnostic gaps that have long hindered effective screening and treatment.
Ultimately, this landmark study echoes a broader call to integrate comprehensive clinical, virological, and pathological data streams, using refined analytical frameworks to safeguard women’s health and reduce the global burden of cervical cancer through smarter, data-driven strategies.
Subject of Research: Assessing risk factors and developing a predictive index combining cytology and endocervical curettage (ECC) to identify undetected cervical cancer in women with biopsy-confirmed high-grade cervical intraepithelial neoplasia.
Article Title: Assessing the risk of undetected cervical cancer in women with a biopsy of high-grade cervical intraepithelial neoplasia: predictive value of cytology and endocervical curettage (ECC)
Article References:
Yao, X., Qie, M., Kang, L. et al. Assessing the risk of undetected cervical cancer in women with a biopsy of high-grade cervical intraepithelial neoplasia: predictive value of cytology and endocervical curettage (ECC). BMC Cancer 25, 1238 (2025). https://doi.org/10.1186/s12885-025-14565-3
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14565-3
Tags: cervical cancer predictionclinical implications of cervical cancer screeningcytology and ECC combinationearly cancer detection methodshidden cervical cancer factorshigh-grade cervical intraepithelial neoplasiaHPV testing limitationsmultivariate logistic regression in oncologypatient outcomes in cervical cancerpredictive value of cytological evaluationsretrospective study on cervical cancerundiagnosed invasive cancers