In a groundbreaking advance that could reshape the future of brain cancer treatment, researchers have developed a cutting-edge data assimilation framework capable of predicting the spatiotemporal response of high-grade gliomas to chemoradiation therapy. High-grade gliomas, notorious for their aggressive nature and invasive spread within the brain, pose considerable challenges in clinical management due to their highly variable responsiveness to standard treatments. This novel computational approach promises to transform personalized treatment planning by providing clinicians with precise, patient-specific forecasts of tumor dynamics throughout the course of therapy.
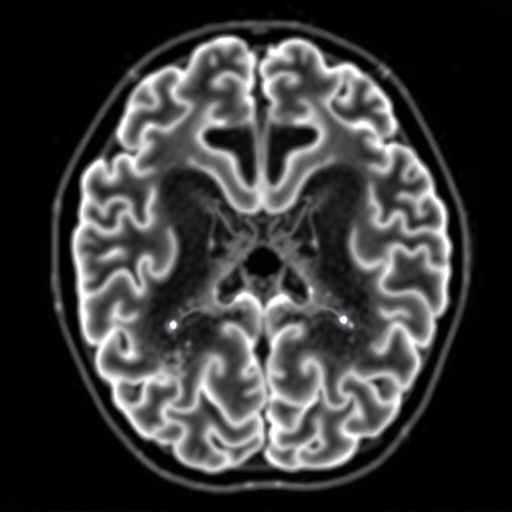
At the heart of this innovation lies a sophisticated two-species reaction-diffusion model that delineates the complex interplay between enhancing and non-enhancing tumor regions. Unlike traditional methods that often rely on static snapshots of tumor size or morphology, this model dynamically integrates serial magnetic resonance imaging (MRI) data to evolve alongside the tumor’s biological behavior. By tracking and simulating both proliferative (enhancing) and non-proliferative (non-enhancing) cellular populations, the framework captures the heterogeneous growth patterns that characterize high-grade gliomas and their differential responses to chemoradiation.
The research team employed a rigorous methodology to validate the accuracy and utility of their model through two distinctive evaluation scenarios. First, they conducted patient-specific calibrations using weekly MRI data collected from 21 individuals undergoing chemoradiotherapy. This frequent and detailed monitoring allowed the assimilation framework to adjust model parameters continuously, refining its predictions in real time as new imaging information became available. The results were remarkable, achieving an exceptionally high concordance correlation coefficient of 0.91 between predicted and observed tumor cell populations, alongside minimal discrepancies in tumor volumetrics.
.adsslot_a3nLCcR8Sv{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_a3nLCcR8Sv{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_a3nLCcR8Sv{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Recognizing the practical limitations of weekly imaging in clinical settings, the researchers explored a second scenario featuring limited data availability. Here, the model was calibrated solely on the initial two imaging visits, with the goal of forecasting tumor evolution for the remaining five weeks of treatment. To optimize predictive performance under these constraints, three parameter assignment strategies were evaluated: reliance purely on individual patient data, integration of cohort-derived averages, or exclusive use of cohort-level parameters. Intriguingly, the study found that incorporating cohort data significantly enhanced prediction accuracy, indicating that while individual patient data is valuable, population-level insights provide a critical scaffold for robust tumor modeling when longitudinal data is sparse.
This pioneering framework’s ability to seamlessly blend personalized imaging data with cohort statistics marks a significant paradigm shift in how oncologists could approach glioma management. By embracing a data-driven, continuously adapting model, clinicians might soon tailor chemoradiation regimens not only based on baseline tumor characteristics but also informed by evolving tumor behavior during therapy. Such adaptive treatment planning holds the promise of maximizing therapeutic efficacy while minimizing unnecessary toxicity.
Importantly, the model also addresses the notorious challenge of tumor heterogeneity—a major obstacle in glioma prognostication. By differentiating between enhancing and non-enhancing tumor compartments, the framework captures subtle biological nuances and spatial variations in treatment response. This granularity allows for more refined predictions of regions at risk for progression or treatment resistance, potentially guiding targeted interventions such as localized dose escalation in radiotherapy or adaptive chemotherapy protocols.
Furthermore, the researchers’ rigorous validation process underscores the robustness and clinical relevance of their approach. The high concordance observed during weekly calibrations reinforces confidence in the model’s capacity to mirror real-world tumor dynamics. Meanwhile, the second scenario’s results highlight a practical avenue for deploying this technology in resource-limited environments or settings with less frequent imaging protocols.
Beyond gliomas, the principles underpinning this data assimilation framework may have broad applicability across oncology and other fields characterized by complex spatiotemporal biological phenomena. Tumors and other pathological entities that exhibit spatial heterogeneity and dynamic evolution could be modeled with similar approaches, heralding a new era of precision medicine powered by continual data integration and computational modeling.
Despite its promising advances, the framework also presents avenues for future enhancements. Integration with multi-modal imaging techniques, such as functional MRI or positron emission tomography (PET), could further enrich model inputs by incorporating metabolic and physiological tumor metrics. Additionally, coupling the model with molecular and genomic tumor profiling might unveil deeper layers of biological complexity, enabling even more nuanced predictions.
The implications of this research extend beyond the technical sphere, potentially influencing clinical trial design, therapeutic decision-making, and patient quality of life. Accurate early predictions of treatment response could identify non-responders sooner, allowing for timely treatment modifications or enrollment in alternative therapeutic protocols. Meanwhile, patients predicted to respond favorably could avoid overtreatment and associated side effects, underscoring the framework’s role in personalized medicine.
As treatment of high-grade gliomas remains one of the most formidable challenges in neuro-oncology, innovations such as this provide a beacon of hope. The integration of advanced computational modeling with longitudinal patient data represents a leap toward more effective, adaptive, and patient-centered therapy. Continued development and clinical translation of such frameworks could ultimately improve survival outcomes and redefine standards of care in this devastating disease.
In conclusion, this study from Miniere et al. delivers a compelling demonstration of how data assimilation strategies can revolutionize tumor growth modeling and prediction in high-grade gliomas. By strategically combining individual patient imaging with broader cohort data, the authors present a practical, scalable solution to forecasting tumor response during chemoradiation. This work not only advances our scientific understanding of glioma biology but also sets the stage for next-generation clinical tools that enhance decision-making and personalize cancer treatment.
The fusion of mathematical modeling, medical imaging, and clinical oncology exemplified by this research holds transformative potential. As computational power and imaging technologies continue to evolve, frameworks like the one described here are poised to become indispensable assets in the fight against aggressive brain tumors. This synergy between data and medicine illustrates the future of precision oncology—where informed predictions guide bespoke therapies for each patient’s unique disease journey.
Subject of Research: High-grade gliomas and their spatiotemporal response to chemoradiation therapy through computational data assimilation models.
Article Title: A data assimilation framework for predicting the spatiotemporal response of high-grade gliomas to chemoradiation.
Article References: Miniere, H.J.M., Hormuth, D.A., Lima, E.A.B.F. et al. A data assimilation framework for predicting the spatiotemporal response of high-grade gliomas to chemoradiation. BMC Cancer 25, 1239 (2025). https://doi.org/10.1186/s12885-025-14557-3
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14557-3
Tags: aggressive brain tumor managementcomputational frameworks in glioma researchenhancing and non-enhancing tumor regionsglioma chemoradiation response predictionheterogeneity in glioma growth patternshigh-grade glioma treatment advancementsMRI data integration for tumor analysispatient-specific cancer treatment planningpersonalized brain cancer therapyreaction-diffusion model in oncologyspatiotemporal tumor dynamics modelingvalidating cancer treatment models