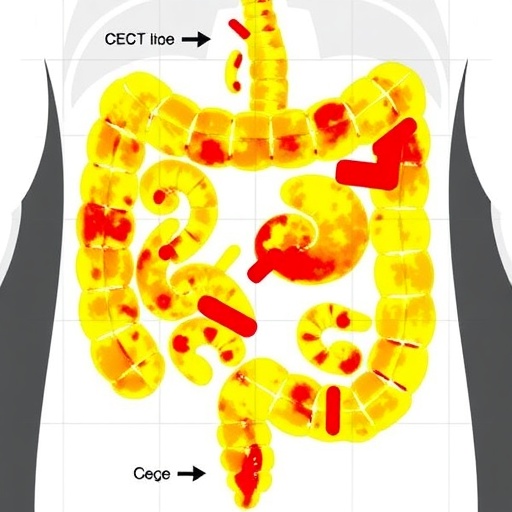
In a significant leap forward for oncological diagnostics, recent research has illuminated the powerful role of contrast-enhanced computed tomography (CECT) combined with clinical profiling in the preoperative prediction and localization of synchronous metastases in colon cancer patients. This groundbreaking study underscores the potential to transform traditional cancer staging protocols, offering a more precise roadmap for treatment and potentially improving survival outcomes.
Colon cancer remains one of the most prevalent malignancies worldwide, and accurate detection of metastases prior to surgical intervention is critical for determining the most appropriate therapeutic strategy. Conventional imaging techniques often struggle to capture the nuanced biological behaviors of metastatic lesions, especially when they occur simultaneously at multiple sites. Addressing this challenge, the study conducted a meticulous retrospective analysis of 212 pathologically verified colon cancer cases, providing a robust dataset for evaluating CECT’s diagnostic prowess.
The patient cohort, composed of nearly equal proportions of males and females with a mean age of 64 years, underwent preoperative CECT within a narrow two-week window prior to surgery. This timeframe ensured the imaging findings closely reflected the tumor biology at the time of intervention. The research team leveraged the complementary expertise of two independent radiologists, who systematically examined tumor enhancement patterns, lesion morphology, and lymph node status, thereby ensuring the reliability and reproducibility of imaging interpretations.
A pivotal aspect of the study was the stratification of distant metastases into precise categories: synchronous liver metastases, peritoneal metastases, and metastases to other anatomical locations. This classification allowed for a tailored analysis of metastatic presentations, acknowledging that the biological behavior and clinical implications vary substantially depending on the metastatic site. The researchers confirmed metastatic disease via tissue biopsy or unmistakable imaging hallmarks, furnishing a solid diagnostic foundation.
One of the most compelling findings was the identification of a suite of independent predictors closely associated with synchronous metastases. Elevated levels of carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9), both established tumor markers, surfaced as significant biochemical harbingers of metastatic spread. Morphometric parameters extracted from the CECT images, such as increased tumor length and the tumor length-to-thickness ratio, revealed insights into tumor aggressiveness and invasion potential, effectively linking radiological features with biological behavior.
Moreover, the presence of tumor necrosis and lymph node necrosis emerged as critical imaging biomarkers of metastatic propensity. Necrotic tissue within primary tumors and lymph nodes may indicate hypoxia, rapid tumor growth, and aggressive phenotypes, which collectively portend poor prognosis. The study further elucidated the diagnostic value of assessing arterial-venous phase CT value differences, a nuanced radiographic parameter reflecting tumor vascularity and perfusion dynamics, which can signify metastatic potential with remarkable sensitivity.
Integrating these diverse predictors, the researchers constructed a sophisticated predictive model that demonstrated impressive diagnostic accuracy, with an area under the receiver operating characteristic curve (AUC) of 0.852. The model’s sensitivity and specificity underscore its practical utility in clinical settings, providing doctors with a powerful tool to stratify patients preoperatively and tailor therapeutic planning accordingly. This approach heralds a shift toward precision medicine in oncology, where individualized risk assessment guides decision-making.
The study also delved into the particular sphere of peritoneal metastases, a notoriously challenging condition to detect due to the subtlety of peritoneal implants on imaging studies. Here, two additional factors—tumor necrosis and the presence of ascites—were strongly linked with peritoneal spread. Ascites, the pathological accumulation of fluid within the abdominal cavity, may facilitate tumor cell dissemination and serve as an indirect but vital imaging clue in evaluating metastatic disease.
Building on these findings, the peritoneal metastasis-focused predictive model achieved even higher predictive values (AUC = 0.869), illustrating the model’s precision in this subgroup of colon cancer patients. The high sensitivity and specificity indicate the potential for earlier intervention, which could ultimately mitigate disease progression and enhance patients’ quality of life. This facet of the research accentuates the clinical significance of integrating imaging biomarkers with biochemical and morphological data.
The implications of this study are profound. By harmonizing clinical and radiological data, healthcare providers can obtain a holistic view of tumor biology and metastatic distribution, enabling the formulation of personalized treatment regimens. Such regimens may include neoadjuvant therapies aimed at shrinking tumors and metastases before surgery, or tailored surgical approaches that comprehensively address metastatic sites, thereby reducing recurrence rates.
Furthermore, this predictive approach can serve as a critical decision-support tool in multidisciplinary tumor boards, fostering collaboration among radiologists, surgeons, oncologists, and pathologists. It bridges traditionally siloed diagnostic modalities, creating a cohesive framework for patient management. Adoption of these predictive models into routine clinical practice could revolutionize colon cancer care pathways globally.
It is worth noting that this research also underscores the pivotal role of advanced imaging techniques in oncology. The ability of CECT to highlight dynamic vascular and tissue characteristics offers insights that transcend mere morphological evaluation. Future research may further refine these imaging biomarkers through the incorporation of radiomics and machine learning algorithms, enhancing predictive accuracy and facilitating automated image analysis.
Moreover, the exploration of tumor necrosis and its association with metastases opens new avenues for targeted therapies. Understanding the molecular underpinnings of necrotic tumor regions may unveil vulnerabilities exploitable by novel pharmacological agents. Similarly, the role of ascites in facilitating tumor dissemination invites further investigation into strategies to mitigate peritoneal spread.
As the burden of colon cancer continues to climb globally, innovations that improve early detection of metastases and enable precise localization are invaluable. This study offers a blueprint for harnessing the synergy between imaging science and clinical biochemistry, setting a precedent for other cancer types where synchronous metastases complicate treatment.
In conclusion, the integration of preoperative CECT imaging with clinical characteristics represents a transformative advance in the management of colon cancer. This approach enhances the clinician’s ability to detect, characterize, and localize synchronous metastases accurately, empowering personalized interventions that could improve patient survival rates and quality of life significantly. The study, soon to be published in BMC Cancer, stands as a testament to the evolving frontier of diagnostic oncology.
Subject of Research: Preoperative prediction and localization of synchronous metastases in colon cancer using contrast-enhanced computed tomography (CECT) combined with clinical characteristics.
Article Title: Preoperative prediction and localization of synchronous metastases in colon cancer: the role of CECT combined with clinical characteristics
Article References: Fan, Y., Yang, R., Shu, Y. et al. Preoperative prediction and localization of synchronous metastases in colon cancer: the role of CECT combined with clinical characteristics. BMC Cancer 25, 1755 (2025). https://doi.org/10.1186/s12885-025-15103-x
Image Credits: Scienmag.com
DOI: 12 November 2025
Tags: cancer staging protocolsclinical profiling in oncologycolon cancer metastases detectioncontrast-enhanced computed tomographydiagnostic imaging techniquesmetastatic lesion localizationpreoperative imaging for cancerradiologist expertise in cancer diagnosticsretrospective analysis of cancer casessurvival outcomes in colon cancertumor biology and treatment strategy