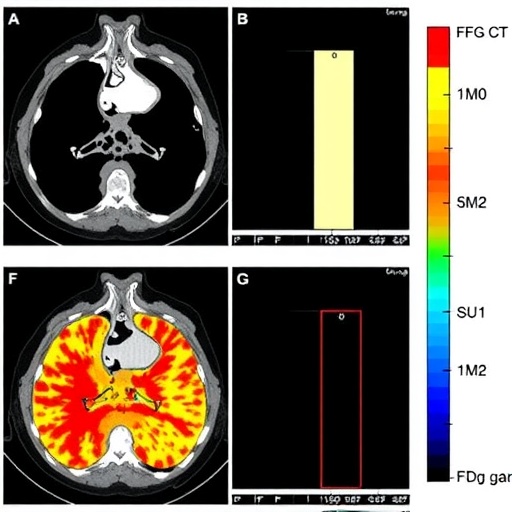
In a groundbreaking study published in BMC Cancer, researchers have offered critical new insights into the predictive capabilities of F-18 fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) scans in patients with locally advanced rectal cancer (LARC) undergoing neoadjuvant chemoradiotherapy (nCRT). Despite the widespread clinical use of FDG PET/CT for oncological staging and response evaluation, the study reveals that baseline metabolic parameters such as maximum standardized uptake value (SUVmax), metabolic tumor volume (MTV), and total lesion glycolysis (TLG) show limited utility in forecasting treatment response and survival outcomes in this patient population.
The research team embarked on a comprehensive retrospective analysis involving 151 patients diagnosed with LARC who received nCRT followed by surgical resection over a nine-year period from 2014 to 2023. Central to their investigation was the correlation between pre-treatment PET/CT metabolic data and tumor regression grade (TRG) post-surgery, categorized according to the Mandard classification system. Patients were dichotomized into complete responders (TRG1) and incomplete responders (TRG2–5), allowing for a focused assessment of clinical and pathological factors influencing outcomes.
Metabolic parameters derived from FDG PET/CT have long been hypothesized as potential biomarkers for tumor behavior and treatment sensitivity. SUVmax, referring to the peak uptake within the tumor, along with volumetric measures such as MTV and TLG, reflect both the metabolic activity and tumor burden. However, intriguingly, the study’s findings contradict expectations, as none of these PET/CT parameters demonstrated statistically significant predictive value for either pathological tumor regression or survival endpoints in the context of neoadjuvant therapy.
.adsslot_n6Ie3HACYO{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_n6Ie3HACYO{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_n6Ie3HACYO{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Instead, attention shifted to a host of clinico-pathological variables that emerged as robust predictors of therapeutic success and prognosis. Family history of cancer, baseline and post-treatment carcinoembryonic antigen (CEA) levels, radiotherapy-associated carbohydrate antigen 19-9 (CA19-9) dynamics, and the presence of concurrent chemotherapy (CC) stood out as critical factors determining complete response rates. These clinical indicators underscore the multifaceted nature of cancer progression and the limitations of relying solely on imaging data for comprehensive patient stratification.
The impact of histopathological features on treatment outcomes cannot be overstated. Perforation, lymphovascular invasion (LVI), and perineural invasion (PNI)—classic markers of aggressive tumor biology—invariably correlated with incomplete response and worse survival profiles. Their inclusion in multivariate analyses reinforced their independent prognostic significance, highlighting that microscopic tumor behavior ultimately governs response to nCRT beyond what can be visualized metabolically.
From a survival perspective, TRG1 patients enjoyed markedly improved overall survival (OS) and disease-free survival (DFS), reflecting the clinical importance of achieving a complete pathological response. Kaplan–Meier survival curves neatly illustrated these disparities, reinforcing TRG1 as a pivotal biomarker for patient prognosis. Moreover, multivariate Cox regression models revealed that TRG1 status, administration of concurrent chemotherapy, and absence of tumor perforation independently predicted improved survival outcomes.
The lack of correlation between pre-treatment FDG PET/CT parameters and treatment response represents a significant paradigm shift. This revelation urges oncologists and radiologists to reconsider the predictive weight traditionally assigned to metabolic imaging in the neoadjuvant setting for rectal cancer. It further emphasizes the necessity of integrating a more holistic clinical and pathological approach when designing personalized treatment strategies.
Neoadjuvant chemoradiotherapy is a cornerstone in managing LARC, frequently enabling tumor downstaging and sphincter-sparing surgeries. However, individualized responses vary greatly, posing challenges to optimizing treatment. The study’s integrative methodology, combining imaging, biochemical markers, and histological data, provides a robust framework that could streamline prognostication and allow for more nuanced clinical decision-making.
CEA and CA19-9, both serum tumor markers, have long been employed in gastrointestinal oncology for monitoring disease progression and recurrence. Their demonstrated associations with TRG and survival in this study reaffirm their clinical utility in tandem with conventional diagnostic tools. Importantly, post-treatment CEA levels emerged as a particularly powerful indicator, reflecting residual tumor burden and potential microscopic disease persistence.
Concurrent chemotherapy, when administered alongside radiotherapy, was associated with better pathological response and improved survival metrics. This finding aligns with existing literature advocating for combination regimens to enhance radiosensitization and maximize tumor eradication. It validates current therapeutic protocols and paves the way for further investigations into optimizing concurrent treatment modalities.
The study also explored the role of family history, traditionally a surrogate for genetic predisposition and shared environmental risk factors, in modulating treatment response. The strong association observed suggests that genetic and epigenetic influences may play a more significant role in therapeutic sensitivity than previously recognized, warranting further molecular profiling studies to elucidate underlying mechanisms.
Importantly, the presence of perforation—an indicator of tumor invasion into surrounding tissues—was strongly predictive of poorer outcomes. This emphasizes the aggressive nature of certain rectal cancers and the need for early detection and intervention. Histopathological assessment after surgery remains indispensable for accurate staging and prognosis.
Perineural invasion and lymphovascular invasion, both indicative of tumor dissemination pathways, independently impacted treatment response and survival, reaffirming their value as critical prognostic factors. Their detection necessitates thorough pathological evaluation to guide adjuvant therapy considerations.
While FDG PET/CT remains invaluable for cancer staging and detecting distant metastases, this study cautions against overreliance on baseline metabolic parameters as solitary prognostic tools in the context of nCRT for LARC. A multimodal diagnostic strategy incorporating serum markers, histopathological examination, and clinical context remains paramount.
The findings presented in this study have profound implications for clinical practice. They suggest that clinicians should place greater emphasis on molecular and histopathological markers when predicting response to nCRT in rectal cancer. Additionally, the study advocates for continued research into novel biomarkers and imaging techniques that might better capture the complexity of tumor biology and treatment effects.
This comprehensive investigation lays the foundation for refining patient selection criteria and tailoring neoadjuvant treatment protocols. By recognizing the limited prognostic role of baseline FDG PET/CT metabolic parameters and amplifying the significance of clinical-pathological features, oncologists can enhance therapeutic precision, improve survival rates, and ultimately advance patient care in rectal cancer management.
Subject of Research: Predictive value of baseline F-18 FDG PET/CT metabolic parameters and clinico-pathological variables in tumor regression and survival outcomes in locally advanced rectal cancer patients undergoing neoadjuvant chemoradiotherapy.
Article Title: Evaluation of pre-treatment F-18 FDG PET/CT according to Mandard classification in locally advanced rectal cancer patients undergoing neoadjuvant chemoradiotherapy.
Article References:
Aras, F., Parvizi, M., Nalbant, O.A. et al. Evaluation of pre-treatment F-18 FDG PET/CT according to Mandard classification in locally advanced rectal cancer patients undergoing neoadjuvant chemoradiotherapy. BMC Cancer 25, 1262 (2025). https://doi.org/10.1186/s12885-025-14659-y
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14659-y
Tags: BMC Cancer research findingsLocally Advanced Rectal CancerMetabolic Tumor Volume AnalysisNeoadjuvant Chemoradiotherapy OutcomesOncological Staging with PET/CTPre-Treatment FDG PET/CTRectal Cancer Response Predictionretrospective study on cancer treatmentSurgical Resection in Rectal CancerSUVmax as a BiomarkerTotal Lesion Glycolysis in CancerTumor Regression Grade Assessment