Clotting cells are also an important regulator of inflammation, reveals study by the University of Bonn
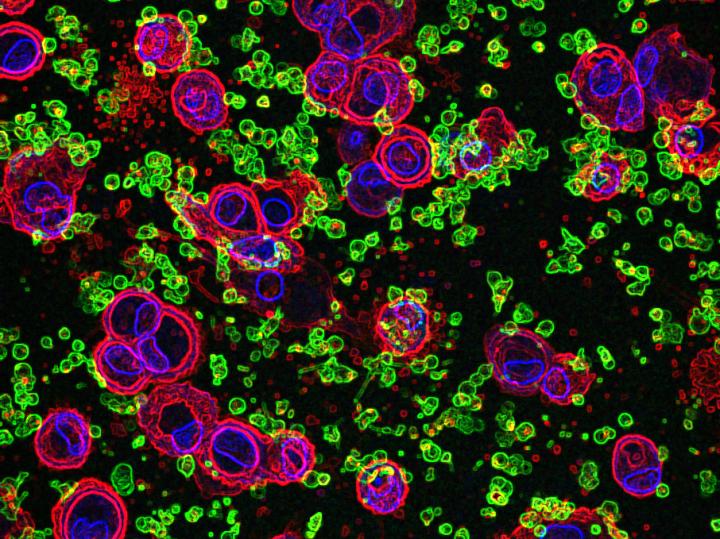
Credit: © artistic representation (based on microscopic images): B. Franklin/L. Ribeiro/UKB
Platelets not only play a key role in blood clotting, but can also significantly intensify inflammatory processes. This is shown by a new study carried out by scientists from the University of Bonn together with colleagues from Sao Paulo (Brazil). In the medium term, the results could open up new ways to treat autoimmune diseases. They have now been published in the renowned journal Cell Reports.
For a long time, the role of platelets appeared to be clear: in the event of an injury, they adhere to the wound and stick to each other to rapidly stop the bleeding. This wound closure mechanism works quickly and efficiently, but its protagonists were not considered to have any other functions.
For some years now, this picture has begun to change significantly: these tiny cells, each of which is about the size of an intestinal bacterium, are also believed to perform important functions in the immune system. The current study by the universities of Bonn and Sao Paulo supports this thesis: it shows that platelets ensure that the white blood cells (the leukocytes) secrete significantly more inflammatory messengers. “It is possible that this effect contributes to the often severe course of autoimmune diseases,” explains Prof. Dr. Bernardo Franklin from the Institute of Innate Immunity at the University Hospital Bonn. “These are diseases in which the immune system attacks and destroys the body’s own tissue.”
In their study, the researchers focused on an important immune mechanism: the activation of the NLRP3 inflammasome. Inflammasomes are molecular machines that consist of a number of different proteins. Among other things, they are able to convert inactive inflammatory messengers into their active form. One of them is the interleukin 1 (IL-1). When cells secrete IL-1, they call on other immune cells to help and thereby trigger a strong inflammatory reaction. As this can also become dangerous for the body, the activity of the inflammasomes, and hence also the formation of IL-1, is strictly regulated.
“We have now been able to demonstrate that platelets interfere with this regulation,” explains Dr. Lucas Ribeiro, first author of the study: “They cause certain white blood cells, the macrophages and neutrophilic granulocytes, to form more active inflammasomes.” To do this, they apparently release a whole cocktail of substances that diffuse to the white blood cells. Once there, these ensure, among other things, that certain genes required for the construction of the inflammasomes are more frequently expressed. This effect does not require the platelets to make direct contact with the macrophages or granulocytes. Instead, they release their active substances into the environment, for example, into the blood.
“To prove that, we incubated human platelets in the laboratory and then filtered them off, so the platelet factor could be present in the culture medium,” explains Dr. Ribeiro. “When we added this platelet medium to human white blood cells, the formation of inflammasomes and the IL-1 production were significantly boosted.” Exactly which of the substances released by the platelets are responsible for this process is not yet known. However, the effect was supported by observations in human malaria patients: the more platelets they have, the higher the IL-1 concentration in their plasma. The researchers also experimentally reduced the number of platelets in mice. The animals then released significantly less IL-1 after being injected with inflammatory compounds.
As IL-1 promotes inflammation, the messenger substance can significantly worsen the course of autoimmune diseases. Nevertheless, Prof. Franklin is keen to speak up against a one-sided view of platelets as villains: they also intervene in other ways in the immune response, for example by preventing the development of life-threatening sepsis after an infection. Regardless of this, the results might pave the way to new therapies for diseases such as rheumatism or diabetes.
Single cell cultures do not tell the whole story
However, one important message of the current study is of a more general nature: isolated blood cells in culture often behave very differently than in their natural environment, where they communicate with numerous other cells. “Experiments in the test tube therefore do not provide complete insight into the processes happening in the body,” emphasizes Prof. Franklin. “Still, most of research into inflammasomes are based on them, which is a fact we should rethink.” After all, platelets may only reveal their additional immune functions in concert with white blood cells.
###
Publication: Verena Rolfes, Lucas Secchim Ribeiro, Ibrahim Hawwari, Lisa Böttcher, Nathalia Rosero, Salie Maasewerd, Marina Lima Silva Santos, Tomasz Próchnicki, Camila Meirelles de Souza Silva, Carlos Wagner de Souza Wanderley, Maximilian Rothe, Susanne V. Schmidt, H. James Stunden, Damien Bertheloot, Magali Noval Rivas, Cor Jesus Fontes, Luzia Helena Carvalho, Fernando de Queiroz Cunha, Eicke Latz, Moshe Arditi and Bernardo Simoes Franklin: Platelets fuel the inflammasome activation of innate immune cells; Cell Reports, DOI: https:/
Contact:
Prof. Dr. Bernardo Franklin
Institute of Innate Immunity
University Hospital Bonn
Tel. +49 228/287-51981
E-mail: [email protected]
Media Contact
Prof. Dr. Bernardo Franklin
[email protected]
Related Journal Article
http://dx.




