In a groundbreaking study, researchers have elucidated the complex interplay between PD-L1 and c-MET, revealing significant insights that could alter treatment approaches in non-small cell lung cancer (NSCLC). The pivotal findings presented by Hsu et al. in their forthcoming publication in the Journal of Biomedical Science address a prevalent challenge in oncology: the development of drug resistance, particularly concerning osimertinib, a targeted therapy for patients with EGFR mutations. The implications of this research extend beyond basic science, holding potential to reshape therapeutic strategies for NSCLC patients facing metastatic disease.
Osimertinib, an irreversible EGFR tyrosine kinase inhibitor (TKI), has transformed the treatment landscape for EGFR-mutant NSCLC, offering improved outcomes over earlier generation TKIs. Despite its efficacy, a substantial number of patients eventually develop resistance to this therapy, predominantly due to bypass signaling pathways and compensatory mechanisms that allow tumor survival. This study focuses on the molecular interactions that contribute to this resistance, particularly the role of PD-L1, a well-known immune checkpoint regulator.
PD-L1’s involvement in the tumor microenvironment has been well-documented, primarily in terms of immune evasion. However, the nuanced role it plays in enhancing the phosphorylation of c-MET—an essential player in cell signaling pathways that promote cancer progression—emerges as a novel dimension in this study. The research demonstrates that PD-L1 does not merely represent a target for immune modulation; rather, it actively participates in the oncogenic signaling cascade, thus facilitating a more aggressive tumor phenotype.
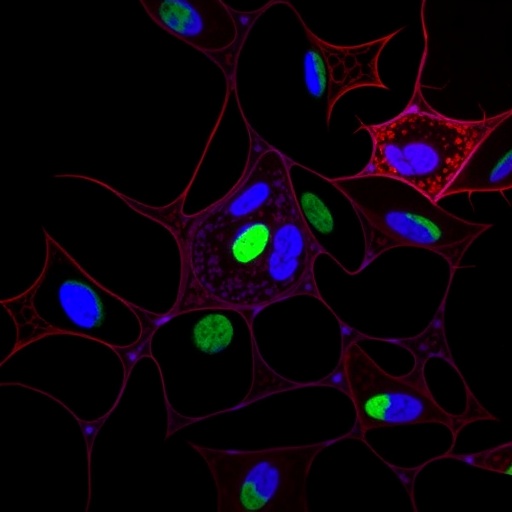
The team utilized a series of in vitro and in vivo experiments to explore how PD-L1 affects c-MET phosphorylation and the downstream effects of this interaction. Through the application of precise molecular techniques and rigorous statistical analyses, they revealed that elevated PD-L1 expression correlates with increased c-MET activity in EGFR-mutant NSCLC cell lines. This relationship highlights a potentially exploitable vulnerability within tumors that could inform future therapeutic interventions, making it imperative to closely monitor PD-L1 levels in clinical settings.
Moreover, the researchers uncovered that the activation of c-MET is not solely a byproduct of oncogenic signaling but is intricately linked to the resistance mechanisms that tumors develop against targeted therapies like osimertinib. The findings suggest that correlative therapies aimed at inhibiting c-MET could potentially resensitize tumors to osimertinib, offering a combinatorial treatment approach that may enhance clinical outcomes for patients who have previously relapsed after EGFR TKI therapy.
The study further expands on the implications of these molecular interactions in terms of the surrounding immune landscape. The interplay between PD-L1 and c-MET occurs within a delicate balance of tumor-immune interactions, where elevated PD-L1 potentially suppresses anti-tumor immunity while simultaneously promoting aggressive tumor characteristics through MET signaling. This dual role complicates treatment strategies, as therapies designed to inhibit PD-L1 may inadvertently destabilize this relationship, leading to unforeseen consequences in terms of tumor evolution and patient response.
As personalized medicine continues to gain traction, these insights emphasize the necessity for oncologists to consider not only the genetic landscape of tumors but also their dynamic interactions with immune evasion mechanisms. The notion that therapies may need to be tailored not only to the presence of specific mutations but also to the expression of key regulatory proteins like PD-L1 poses exciting challenges for the field. Future research should focus on the development of dual-targeting strategies that simultaneously inhibit PD-L1 and c-MET, thereby tackling the resistance pathways head-on.
In conclusion, the research conducted by Hsu et al. provides a crucial foundation for understanding the multifaceted role of PD-L1 in c-MET signaling and its implications for resistance to osimertinib. The findings underscore the urgency for clinical trials aimed at combining PD-L1 inhibitors with c-MET antagonists, which may hold the key to overcoming one of the most significant obstacles in the treatment of EGFR-mutant NSCLC. By further investigating these pathways, the scientific community may unlock innovative approaches that not only combat resistance but also improve survival and quality of life for patients grappling with this formidable disease.
As we navigate through this intricate landscape of cancer biology, it is vital to remember that each discovery brings us closer to the development of more effective therapies. The insights provided by this study represent a stepping stone toward a future where we can not only understand but also strategically manipulate the tumor microenvironment for better patient outcomes. As we await further research and clinical validation, this study stands as a testament to the innovative spirit of contemporary cancer research.
The challenges of NSCLC remain daunting, but with the continued exploration of the molecular dynamics at play, there is hope that we can turn the tide in the battle against this cancer. As therapeutic advancements arise from such pivotal studies, they could pave the way for a new era in lung cancer treatment, characterized by enhanced precision and efficacy.
The study’s contribution to the body of knowledge surrounding PD-L1 and c-MET is profound, highlighting a critical intersection of immunology and oncology. It calls for a collective effort to bridge the gap between laboratory discoveries and clinical application, ensuring that patients benefit from the rapidly evolving landscape of cancer therapeutics.
In closing, the research by Hsu and colleagues provides a vital framework for future exploration and reinforces the idea that our approach to cancer treatment must continue to evolve. By embracing the complexity of tumor biology, we can develop the strategies needed to surmount resistance and improve outcomes for patients with EGFR-mutant NSCLC.
Subject of Research: Interaction between PD-L1 and c-MET in EGFR-mutant NSCLC and its implications for osimertinib resistance.
Article Title: PD-L1 regulates c-MET phosphorylation and contributes to MET-dependent resistance to osimertinib in EGFR-mutant NSCLC.
Article References: Hsu, CC., Huang, D.DR., Hsu, WH. et al. PD-L1 regulates c-MET phosphorylation and contributes to MET-dependent resistance to osimertinib in EGFR-mutant NSCLC. J Biomed Sci 32, 94 (2025). https://doi.org/10.1186/s12929-025-01181-3
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12929-025-01181-3
Keywords: NSCLC, PD-L1, c-MET, osimertinib, EGFR-mutant, drug resistance, cancer therapy.
Tags: c-MET signaling in cancer progressiondrug resistance in oncologyEGFR mutation targeted therapyHsu et al. biomedical research findingsimplications for metastatic lung cancer treatmentmolecular pathways in cancernon-small cell lung cancer treatmentnovel therapeutic strategies for NSCLCosimertinib resistance mechanismsPD-L1 and c-MET interactionPD-L1 phosphorylation effectstumor microenvironment and immune evasion