COLUMBUS, Ohio — In a revolutionary breakthrough that could dramatically reshape the future of cancer immunotherapy, researchers at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James) have unveiled a novel cellular mechanism underlying T cell exhaustion. This in-depth study uncovers how stress responses linked to protein misfolding plunge T cells into a dysfunctional state, profoundly impairing their anti-tumor activity and immune surveillance capabilities. The innovative findings suggest new therapeutic targets to rejuvenate exhausted T cells and significantly boost the efficacy of cancer immunotherapies by modulating the protein production cycle.
This investigation stems from addressing a long-standing mystery in immunology: the precise causes behind T cell exhaustion, a state where T cells lose their capacity to effectively combat cancer cells despite persistent antigen exposure. Exhausted T cells display diminished proliferation, reduced cytokine production, and attenuated cytotoxicity, making them a considerable bottleneck in the success of current immunotherapies such as checkpoint inhibitors and engineered T-cell treatments. Until now, research focused predominantly on genetic, metabolic, and epigenetic factors, leaving gaps in understanding the protein homeostasis dimension of exhaustion.
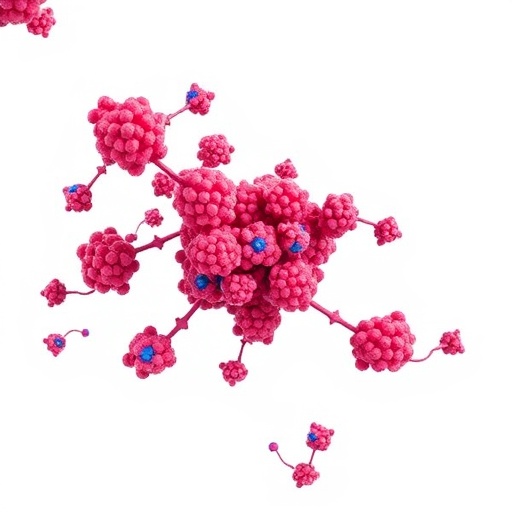
By employing advanced preclinical cancer models, the Ohio State team identified a previously uncharted proteotoxic stress response pathway—termed TexPSR (proteotoxic stress response in T-cell exhaustion)—that decisively contributes to T cell dysfunction. Unlike canonical cellular stress responses that downregulate protein synthesis to mitigate cellular damage, TexPSR paradoxically accelerates protein synthesis. This runaway production leads to an accumulation of misfolded proteins, stress granules, and cytotoxic aggregates reminiscent of neuropathological amyloid plaques observed in Alzheimer’s disease, ultimately overwhelming the cell’s quality control systems.
The consequences of TexPSR activation within exhausted T cells are profound. The relentless buildup of aberrant protein species triggers a collapse of the cellular machinery responsible for target recognition and cytolytic function. This proteotoxic environment effectively “poisons” the T cells, rendering them incapable of attacking tumor cells and enabling immune evasion by the cancer. Notably, the research highlights how TexPSR represents an intrinsic feedback loop that perpetuates exhaustion, suggesting that breaking this cycle could restore T cell competence.
Leading immunological journals, including Nature Reviews Immunology, have described this phenomenon as a “proteotoxic shock,” emphasizing its disruptive impact on T cell fate and tumor immunity. Confirming the translational relevance of their discovery, the OSUCCC – James team demonstrated that pharmacological inhibition of key molecular drivers in the TexPSR pathway rejuvenates exhausted T cells in preclinical tumor models. Therapeutically, this reactivation significantly enhances the potency of existing immunotherapies, showcasing a promising avenue for overcoming treatment resistance in diverse cancers.
Senior author Dr. Zihai Li, an expert in protein folding and immunological research for over thirty years and founding director of the Pelotonia Institute for Immuno-oncology (PIIO), underscored the broader implications of these findings. He states, “T-cell exhaustion has been the primary roadblock in cancer immunotherapy advancement. Our report reveals an unexpected yet pivotal role of protein quality control in this process, opening a new frontier in engineered immunotherapeutics.” Dr. Li, also serving as Deputy Director for Translational Research at OSUCCC – James, emphasized that by illuminating this proteotoxic mechanism, researchers worldwide can strategize novel interventions beyond genetics and metabolism.
Further validating the clinical relevance of TexPSR, the researchers analyzed patient-derived T cells and observed a strong correlation between high TexPSR levels and poor clinical responses to immune checkpoint inhibitors. This insight suggests that TexPSR pathway components could evolve into biomarkers for predicting patient outcomes and tailoring personalized immunotherapy regimens. Moreover, therapeutic targeting of proteotoxic stress offers a tangible strategy to counteract immune evasion tactics employed by malignancies.
First author Yi Wang, a doctoral candidate within Dr. Li’s laboratory, described the destructive cycle uncovered: “Exhausted T cells remain actively producing immune molecules, but those weapons are defective and subsequently destroyed before execution. This autocatalytic degradation impairs immune defense and facilitates tumor persistence.” These mechanistic insights unravel a critical dimension of T cell biology that had remained invisible in prior models, paving the way for innovative therapeutic designs.
The robustness of the TexPSR mechanism was validated across multiple cancer types—including lung, bladder, liver cancers, and leukemia—through extensive preclinical and clinical datasets, affirming its universal relevance. This breadth of application highlights TexPSR’s potential as a foundational target for a wide spectrum of malignancies, where reinvigorating T cells could overcome entrenched therapeutic resistance and improve patient survival.
Published in the prestigious journal Nature, this landmark paper stands as a beacon for the immuno-oncology community, illuminating an unappreciated vulnerability in cancer immunity. The findings herald a paradigm shift: reprogramming the protein quality control pathways in T cells as a critical axis for combating exhaustion and augmenting immunotherapy effectiveness. As the research progresses toward clinical translation, these insights promise to inspire novel drug development pipelines focused on proteostasis and immune resilience.
For additional information about the Pelotonia Institute for Immuno-oncology and ongoing research, visit cancer.osu.edu/PIIO. The study’s DOI is 10.1038/s41586-025-09539-1.
Subject of Research: T cell exhaustion mechanisms and cancer immunotherapy
Article Title: Proteotoxic stress response drives T cell exhaustion and immune evasion
News Publication Date: October 1, 2025
Web References: OSUCCC James, Pelotonia Institute for Immuno-oncology, Nature Article
References:
Li, Z., Wang, Y., et al. Proteotoxic stress response drives T cell exhaustion and immune evasion. Nature. October 1, 2025. DOI: 10.1038/s41586-025-09539-1
Keywords: Cancer immunology, Immune response, Immune cells, Immune system, Immunotherapy
Tags: cancer immunotherapy challengescellular stress responses in immunologycheckpoint inhibitors limitationsengineered T-cell therapy advancementsenhancing anti-tumor activityimmune surveillance and cancer treatmentOhio State University cancer researchprotein misfolding and immune responseprotein quality control in T cellsT cell exhaustion mechanismstherapeutic targets for T cell rejuvenationunderstanding protein homeostasis in T cells