In the relentless pursuit of precision oncology, a groundbreaking study has emerged from an international consortium of researchers, unveiling a pioneering long noncoding RNA (lncRNA)-based serum signature that forecasts therapeutic response in HER2-positive metastatic breast cancer. This innovative biomarker model specifically predicts benefit from ado-trastuzumab emtansine (T-DM1), a sophisticated antibody-drug conjugate (ADC) that has transformed the therapeutic landscape for patients with this aggressive cancer subtype. The scientific community has long grappled with the challenge of anticipating which patients will derive maximal benefit from targeted therapies like T-DM1, and this study marks a significant step forward by harnessing the untapped potential of circulating lncRNAs.
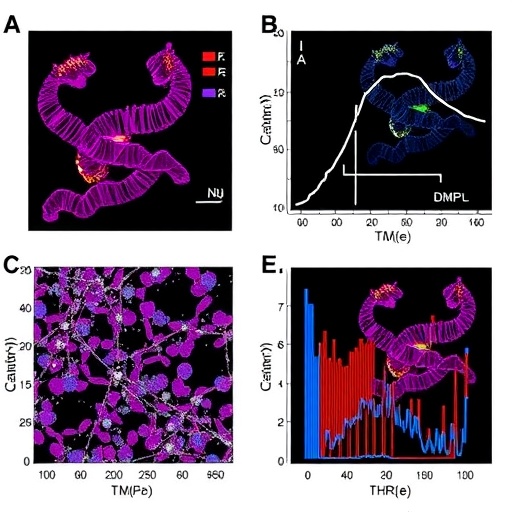
Breast cancer remains the most commonly diagnosed malignancy among women worldwide, with the HER2-positive subset representing a particularly virulent form characterized by human epidermal growth factor receptor 2 overexpression. While trastuzumab and its derivatives, especially T-DM1, have shown remarkable clinical efficacy, heterogeneity in treatment response has limited their universal success. The study in question conducted a multicenter cohort analysis leveraging serum specimens from metastatic breast cancer patients to develop a robust non-invasive prognostic tool. By integrating cutting-edge transcriptomic profiling and rigorous bioinformatic analytics, the research delineated a distinct lncRNA expression profile that correlates strongly with T-DM1 therapeutic outcomes.
Long noncoding RNAs — RNA transcripts longer than 200 nucleotides that do not encode proteins — have emerged as important regulators of gene expression and epigenetic modification, shaping tumor biology and microenvironmental interactions in complex ways. Their stability in biofluids like serum and plasma makes them attractive biomarker candidates, yet clinical translation has been hindered by the complexity of their expression patterns and functional diversity. This study overcame these technical barriers by utilizing comprehensive sequencing technologies to enumerate a specific panel of lncRNAs circulating in the blood of HER2+ metastatic breast cancer patients prior to T-DM1 administration. The resultant signature served not only as a predictor of therapeutic efficacy but also shed light on underlying resistance mechanisms.
Ado-trastuzumab emtansine operates through a precise dual mechanism: the trastuzumab moiety targets HER2 receptors on tumor cells, facilitating internalization, while the emtansine component delivers a cytotoxic payload that disrupts microtubule assembly, triggering apoptosis. Despite this elegant construct, not all HER2-overexpressing tumors respond uniformly, underscoring the need for biomarkers that accurately stratify patients and guide personalized treatment regimens. The lncRNA panel identified showed remarkable sensitivity and specificity when validated across two independent patient cohorts, outperforming conventional predictors like HER2 receptor quantification or other serum protein markers.
This research harnessed advanced machine learning algorithms to refine the predictive model, incorporating patient demographic data, clinical parameters, and lncRNA expression levels to achieve a holistic and actionable signature. Subsequent analyses revealed that patients classified as “high signature score” exhibited significantly prolonged progression-free survival and overall survival following T-DM1 treatment compared to low-score counterparts. Intriguingly, the lncRNA components implicated in the signature are associated with pathways governing cellular proliferation, drug efflux, and immune modulation, providing plausible biological underpinnings for their predictive capacity.
The multicenter design of the study, encompassing diverse patient populations from different geographic regions, enhances the generalizability and translational potential of the findings. Serum samples were meticulously collected and processed under standardized protocols, ensuring reproducibility and minimizing pre-analytical variability. The team’s rigorous validation steps incorporated cross-validation and independent cohort testing, critical prerequisites for clinical adoption. Such methodological stringency addresses a major criticism of prior biomarker studies plagued by small sample sizes and single-center limitations, positioning this signature as a frontrunner for imminent clinical assay development.
Beyond its immediate clinical implications, the study offers expansive insights into the role of lncRNAs as key orchestrators of tumor evolution and therapeutic resistance. Incorporating genomic instability and tumor immune microenvironment parameters, the authors hypothesize that the identified lncRNAs may influence the expression of efflux transporters such as ABC transporters and modulate immune checkpoint pathways, thus affecting both drug intracellular accumulation and immune-mediated tumor clearance. Future functional studies exploring these mechanistic links could not only deepen understanding of cancer biology but also illuminate novel therapeutic targets.
The accessibility of a blood-based predictive tool cannot be overstated in its significance. Traditional tissue biopsies are invasive, fraught with technical limitations, and may not capture tumor heterogeneity or dynamic changes over time. A serum-derived lncRNA signature permits facile and repeated sampling, enabling real-time monitoring of treatment efficacy and early detection of resistance. In the era of evolving precision medicine, such fluid biomarkers are invaluable for tailoring treatment plans that maximize efficacy while minimizing unnecessary toxicity.
Importantly, this study adds to an expanding body of literature positioning lncRNAs as critical regulatory elements beyond coding regions of the genome, challenging the long-held dogma that noncoding RNA serves merely as “junk.” With technological advancements in RNA sequencing and bioinformatics, the once cryptic transcriptome is now revealing layers of complexity and therapeutic relevance previously unappreciated. The convergence of these fields fosters a new paradigm in oncology research and patient care.
Clinicians and oncologists eagerly await the integration of this biomarker into routine clinical workflows, which promises to streamline decision-making processes and improve patient stratification for T-DM1 therapy. By selectively identifying candidates predisposed to benefit, healthcare systems can optimize resource allocation and ameliorate patient outcomes. This aligns with broader objectives to reduce overtreatment and associated adverse events, a critical concern in metastatic disease management.
Critically, this study also underscores the importance of collaborative, multi-institutional research efforts to generate large-scale, high-quality datasets that fuel innovations. The combined expertise of molecular biologists, bioinformaticians, oncologists, and statisticians culminated in a model that transcends the limitations of single-discipline approaches. Such interdisciplinary frameworks set new standards for biomarker discovery workflows.
Looking toward the future, additional longitudinal studies are necessary to assess the durability of this lncRNA signature over multiple treatment cycles and its applicability to other HER2-targeted therapies. Integration with other omics data—such as proteomics, metabolomics, and single-cell transcriptomics—could further refine predictive accuracy. Moreover, exploring the dynamic interplay between tumor-derived lncRNAs and the host immune system may unravel novel immunotherapeutic avenues.
In conclusion, the identification of a serum-based long noncoding RNA signature predicting T-DM1 benefit heralds a new chapter in personalized oncology for HER2-positive metastatic breast cancer. Beyond enhancing patient selection and treatment optimization, these findings reinforce the transformative potential of noncoding RNA biology in reshaping cancer diagnostics and therapeutics. As the field accelerates toward routine clinical implementation, this study represents a beacon of hope for improved survival and quality of life in this challenging patient population.
Subject of Research: Long noncoding RNA-based serum biomarkers predicting ado-trastuzumab emtansine (T-DM1) treatment benefit in HER2-positive metastatic breast cancer.
Article Title: A long noncoding RNA-based serum signature predicts ado-trastuzumab emtansine (T-DM1) treatment benefit in HER2+ metastatic breast cancer patients: a multicenter cohort study.
Article References:
Islam, S.S., Al-Tweigeri, T., Tulbah, A. et al. A long noncoding RNA-based serum signature predicts ado-trastuzumab emtansine (T-DM1) treatment benefit in HER2+ metastatic breast cancer patients: a multicenter cohort study. Cell Death Discov. 11, 421 (2025). https://doi.org/10.1038/s41420-025-02701-8
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02701-8
Tags: antibody-drug conjugate efficacycirculating lncRNAs in cancerHER2-positive breast cancerheterogeneity in breast cancer treatmentinternational cancer research collaborationmetastatic breast cancer prognosisnon-invasive cancer biomarkersnoncoding RNA signatureprecision oncology biomarkersprognostic tools for cancer therapyT-DM1 therapeutic responsetranscriptomic profiling in oncology