Study will compare delamanid to isoniazid for preventing TB disease in at-risk contacts
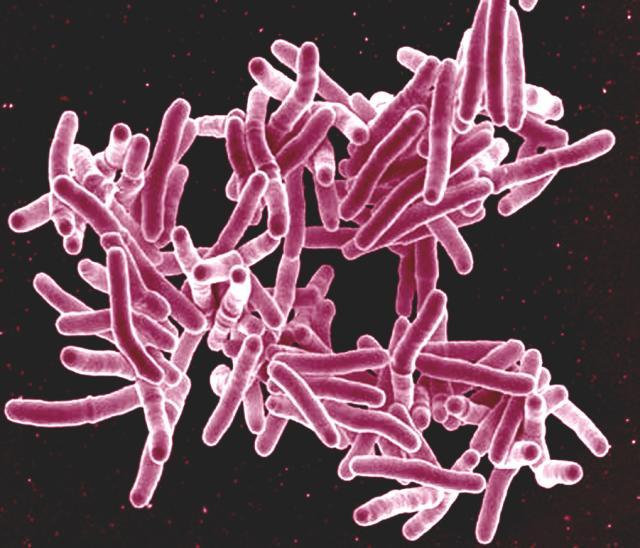
Credit: NIAID
A large clinical trial to assess treatments for preventing people at high risk from developing multidrug-resistant tuberculosis (MDR-TB) has begun. The study is comparing the safety and efficacy of a new MDR-TB drug, delamanid, with the decades-old TB drug isoniazid for preventing active MDR-TB disease in children, adolescents and adults at high risk who are exposed to adult household members with MDR-TB. Study participants are at high risk for MDR-TB because they either have latent TB infection, immune systems suppressed by HIV or other factors, or are younger than age 5 years and therefore have a weak immune system.
Most household members of people with MDR-TB are likely to acquire latent TB infection, in which the bacterium Mycobacterium tuberculosis lives in the body without making a person sick. Without adequate preventive care, many of these individuals will progress to active MDR-TB disease, in which the bacteria become active and multiply. An estimated 460,000 people globally developed MDR-TB in 2017, according to the World Health Organization.
Existing treatments for MDR-TB are often highly toxic and poorly tolerated, placing patients at high risk of disability and death and curing them only about half the time. Treatment options are limited and expensive, and recommended medicines are not always available. Moreover, TB kills more people each year than any other infectious disease. For all these reasons, it is essential to prevent latent TB infection from progressing to active MDR-TB disease.
“It is important to perform randomized, controlled clinical trials on how best to provide preventive care for people who come in close contact with individuals with MDR-TB, since this is a major gap in global public health policy,” said Anthony S. Fauci, M.D. “This new clinical trial will help fill that gap and hopefully define a way to avert much suffering, disability and death from MDR-TB.” Dr. Fauci directs the National Institute of Allergy and Infectious Diseases (NIAID), which is co-funding the study and is part of the National Institutes of Health.
Delamanid is one of the first drugs available specifically to treat people with MDR-TB and the first to exist in a formulation suitable for children. The study investigators hypothesize that prophylactic treatment with delamanid will prove better than isoniazid at reducing the likelihood that at-risk household members of individuals with MDR-TB will develop active TB disease. Isoniazid is the standard drug for TB prevention in many of the study’s host countries.
The Phase 3 clinical trial is called PHOENIx MDR-TB, short for Protecting Households on Exposure to Newly Diagnosed Index Multidrug-Resistant Tuberculosis Patients. The study is co-funded by NIAID and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, also part of NIH. The AIDS Clinical Trials Group (ACTG) and the International Maternal Pediatric Adolescent AIDS Clinical Trials (IMPAACT) Network, both funded by NIH, are conducting the PHOENIx MDR-TB study. The manufacturer of delamanid, Otsuka Pharmaceutical Co., Ltd. of Tokyo, is donating the drug to the trial.
Leading the study are Gavin Churchyard, M.B.B.Ch., M.Med., Ph.D., founder and chief executive officer of the Aurum Institute for Health Research in Johannesburg; Amita Gupta, M.D., M.H.S., deputy director of the Center for Clinical Global Health Education and associate professor of medicine and international health at Johns Hopkins University in Baltimore; Anneke Hesseling, M.D., Ph.D. director of the Desmond Tutu TB Centre in Cape Town, South Africa and distinguished professor in Paediatrics and Child Health at Stellenbosch University, South Africa; and Susan Swindells, M.B.B.S., professor of internal medicine and medical director of the Specialty Care Clinic at the University of Nebraska Medical Center in Omaha.
“We urgently need to halt the spread of MDR-TB,” said Dr. Churchyard, who also chairs the ACTG Tuberculosis Transformative Science Group. “Preventing latent MDR-TB from progressing to active disease protects the health of the individual while reducing the transmission of drug-resistant Mycobacterium tuberculosis.”
The PHOENIx MDR-TB study will take place at more than 27 sites in at least 12 countries, including Botswana, Brazil, Haiti, India, Kenya, Peru, the Philippines, South Africa, Tanzania, Thailand, Uganda and Zimbabwe. The study team will enroll approximately 5,610 participants, including 2,158 adults ages 18 and older who are being treated for confirmed active MDR-TB through their country’s national TB treatment program and 3,452 members of their households who are at high risk for developing active TB disease. The participating household members will be assigned at random to receive either oral delamanid daily for 26 weeks or oral isoniazid plus vitamin B6 daily for 26 weeks. All at-risk members of the same household will receive the same drug regimen.
Both delamanid and isoniazid have minimal potential for interacting with the antiretroviral drugs used to treat HIV. TB is the leading cause of death among people with HIV, according to UNAIDS, causing about one-third of all AIDS-related deaths.
Every 2 to 12 weeks, participating household contacts will visit the study clinic to undergo a physical exam and other health assessments, such as an electrocardiogram, testing of bodily fluids, or a questionnaire. The study team will follow participants for 96 weeks to see if they are protected from active TB disease. Final results from the trial are expected in 2024.
“A highly effective preventive TB therapy for vulnerable household members of people with active MDR-TB disease would be a game-changer in TB care,” said Dr. Hesseling, who chairs the IMPAACT Network’s Tuberculosis Scientific Committee.
The PHOENIx MDR-TB study participants with HIV who have not yet begun treatment for the virus are being referred to local health care providers for antiretroviral therapy, and the study team is documenting participants’ linkage to HIV care.
For more information about the PHOENIx MDR-TB trial, go to ClinicalTrials.gov and search using study identifier NCT03568383.
NIAID supports and conducts basic, translational and clinical research to better understand TB and expedite the development of innovative new tools and strategies to improve TB diagnosis, prevention and treatment. The NIAID Strategic Plan for Tuberculosis Research builds on current research efforts by furthering the understanding of TB and by developing and applying cutting-edge tools to fight the disease.
NIAID conducts and supports research–at NIH, throughout the United States, and worldwide–to study the causes of infectious and immune-mediated diseases, and to develop better means of preventing, diagnosing and treating these illnesses. News releases, fact sheets and other NIAID-related materials are available on the NIAID website.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit http://www.
###
Media Contact
Laura S. Leifman
[email protected]




