Dr. Vanessa Bellat, an assistant professor of chemistry in radiology and an affiliate of the Molecular Imaging Innovations Institute (MI3) at Weill Cornell Medicine, has been awarded a $2 million, four-year R37 MERIT grant from the National Cancer Institute, part of the National Institutes of Health. She will be developing a new therapeutic approach using nanofibers that selectively deliver drugs to the lungs to treat metastatic tumors and testing it in preclinical models. These fibers are made from peptide chains (building blocks that make up proteins) and have a unique 2-dimensional single layer structure that can carry imaging agents and therapeutics.
Credit: Weill Cornell Medicine
Dr. Vanessa Bellat, an assistant professor of chemistry in radiology and an affiliate of the Molecular Imaging Innovations Institute (MI3) at Weill Cornell Medicine, has been awarded a $2 million, four-year R37 MERIT grant from the National Cancer Institute, part of the National Institutes of Health. She will be developing a new therapeutic approach using nanofibers that selectively deliver drugs to the lungs to treat metastatic tumors and testing it in preclinical models. These fibers are made from peptide chains (building blocks that make up proteins) and have a unique 2-dimensional single layer structure that can carry imaging agents and therapeutics.
“I am excited to receive this very competitive grant which allows me to follow my passion for nanotechnology. I believe in the huge potential of nanofibers to revolutionize drug delivery for not only cancer, but other diseases as well,” Dr. Bellat said. “There’s a lot of work to do before bringing it to patients, so this support, which can be extended an additional two years, will help me push this research forward.”
The MERIT program, a backronym for “Method for Extending Research In Time,” gives highly accomplished and promising early career investigators longer-term grant support.
Treating Cancer While Sparing Healthy Cells
Dr. Bellat is focusing on tumors that originated from triple-negative breast cancer and spread to the lungs. Currently, there are no effective treatments for such metastatic lung tumors, which are highly aggressive, complex and genetically diverse. Chemotherapy which kills any fast-growing cells in the body—both healthy and cancerous—is used in clinics in palliative care to prolong a patient’s life, but with severe side effects. Alternative proposed treatments such as targeted therapy and immunotherapy have also failed to successfully treat lung metastases, since these treatments don’t last at the tumor site and often accumulate in off-target organs.
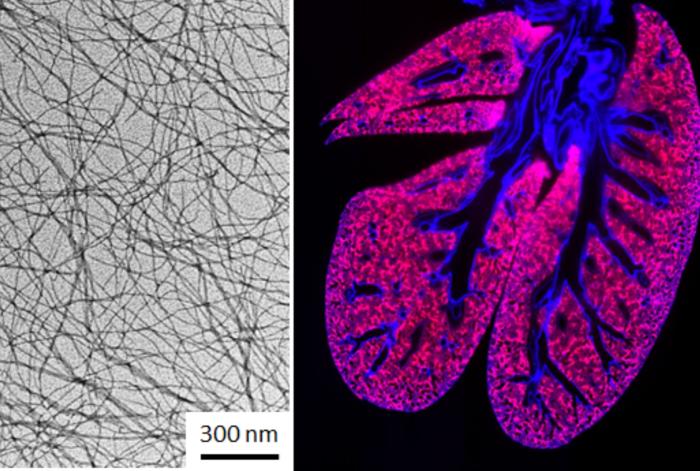
To address the need for improved precision drug-delivery systems that reduce off-target effects, Dr. Bellat’s lab is designing peptide-based nanofibers (pNFP6) that can specifically target and accumulate at the organ of interest. She is using this approach to deliver chemotherapeutic drugs directly to metastatic lung tumors without affecting the rest of the body. The lung-targeting nanofibers are about 10,000 nanometers long, 5 nanometers wide and the thickness is negligible. In comparison, a strand of human hair is 80,000 – 100,000 nanometers wide.
Using pNFP6 for drug delivery is innovative as multiple nanofibers can self-assemble into a large, interconnected network (interfibril) that stays in the lungs, releasing a broad-spectrum of anticancer drugs over time and providing a long-term treatment. The nanofibers are eventually processed by the liver and eliminated from the body much like other drugs. Dr. Bellat’s lab is using the peptide-based nanofiber drug delivery technology in combination with radiation therapy to directly kill cancer cells and activate the body’s immune system. Together, the two approaches could cooperatively and synergistically stop disease progression to provide a more effective treatment.
Tracking Drug Delivery in Real Time
For proof-of-principle studies, Dr. Bellat’s lab will optimize the structure of the nanofibers to carry and release the drug doxorobucin (Dox) only when they reach the tumor microenvironment, which avoids harming healthy tissue. The researchers will also assess the therapeutic efficacy (tumor inhibition and survival benefit) and the toxicity profile of this combination therapy in preclinical models bearing metastatic lung tumors. They can track drug delivery, release and tumor uptake in real time using multiple imaging and microscopic techniques.
“The physical and chemical properties of the nanofibers can be fine-tuned including the size, shape, ability to dissolve in water and surface charges. In doing so, we can control the targeting and retention profile of the nanofibers to treat other cancers, which we are also working on, such as bladder and kidney cancers,” Dr. Bellat said.
For this research, Dr. Bellat will be collaborating with Dr. Benedict Law, associate professor of pharmacology in radiology at Weill Cornell Medicine, and Dr. Claire Vanpouille-Box, assistant professor of cell biology in radiation oncology at Weill Cornell Medicine.



