In a groundbreaking revelation poised to reshape our understanding of liver health, researchers at Mayo Clinic have discerned a critical molecular mechanism detailing how excessive alcohol intake accelerates the progression of fatty liver disease. Fatty liver disease, also medically recognized as Metabolic Dysfunction Associated Steatotic Liver Disease (MASLD), affects over a third of the American population and is a silent precursor to debilitating conditions such as type 2 diabetes and liver cancer. While alcohol’s role in liver damage has been known, this new study precisely elucidates the intricate biochemical processes through which alcohol disrupts cellular maintenance in hepatocytes, the liver’s primary functional cells.
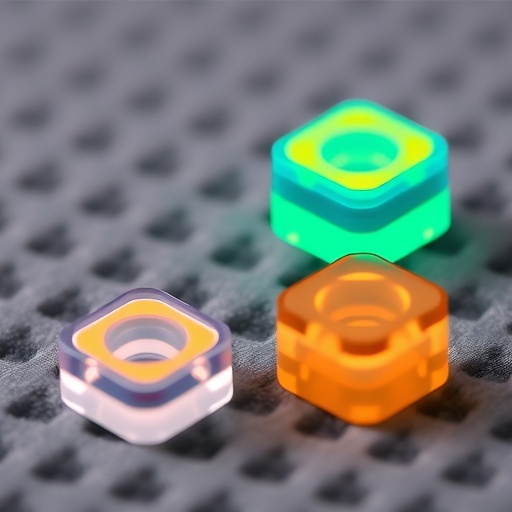
Central to this discovery is the enzyme valosin-containing protein (VCP), an essential molecular machine that orchestrates protein recycling within cells. Under normal physiological conditions, VCP ensures cellular homeostasis by identifying and removing proteins that have become dysfunctional or superfluous. Hepatocytes rely heavily on this system to manage lipid droplets—spherical fat storage organelles that serve as crucial energy reserves during metabolic stress such as fasting. However, when lipid droplets accumulate excessively, a pathological state known as hepatic steatosis or fatty liver ensues, severely impairing liver function.
The research, meticulously led by Dr. Mark McNiven and his team, uncovering VCP’s unanticipated role in regulating a specific protein named HSD17β13, provides substantial insights. HSD17β13 anchors on the surface of lipid droplets, and in healthy liver cells, its levels are tightly controlled by VCP-mediated degradation pathways. It was startling to observe that VCP directly engages with HSD17β13, removing it from lipid droplets and ferrying it to the lysosome, an intracellular organelle responsible for breaking down unwanted protein aggregates. This surveillance mechanism curtails the unchecked expansion of lipid droplets, maintaining cellular lipid equilibrium.
However, exposure to excessive ethanol—the active ingredient in alcoholic beverages—severely impairs this protective mechanism. The study reveals that alcohol effectively dislodges VCP from the lipid droplet surface, nearly eradicating its presence and thus incapacitating its regulatory duties. This loss precipitates an abnormal buildup of HSD17β13 on lipid droplets, triggering an increase in fat storage within hepatocytes. As lipid droplets balloon in size and number due to this protein accumulation, the liver’s architecture and function begin to deteriorate, setting the stage for fatty liver disease progression.
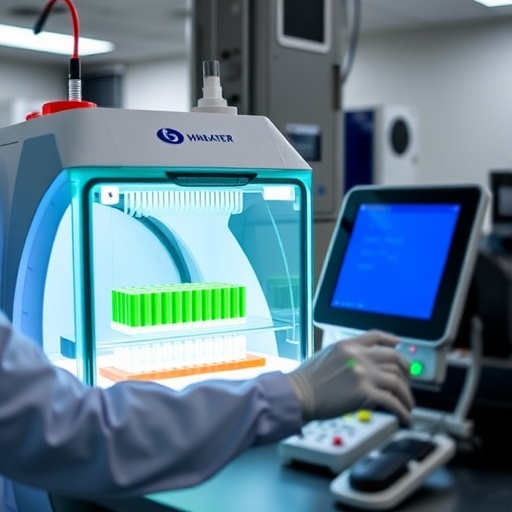
What makes these findings particularly compelling are the live cellular imaging experiments that captured VCP’s recycling choreography in unprecedented detail. The researchers visualized VCP in collaboration with chaperone proteins shepherding HSD17β13-laden lipid droplets towards the lysosome for degradation. This dynamic interplay underscores a finely tuned homeostatic circuit vulnerable to disruption by alcohol metabolites. The research team’s corroborative experiments unambiguously demonstrated that ethanol exposure cripples this cellular quality control system, shedding light on the molecular vulnerability that predisposes certain individuals to alcohol-associated liver damage.
This pivotal insight holds transformative implications not only for understanding disease etiology but also for therapeutic innovation. By identifying HSD17β13 as a potential drug target, the study lays the foundation for novel interventions aimed at modulating lipid droplet dynamics and preventing or reversing steatosis. Targeted therapies could conceivably restore or mimic VCP’s function, reestablishing the lysosomal degradation of excess HSD17β13 and arresting fatty liver disease at its nascent stage.
Moreover, these findings enrich the broader scientific narrative surrounding lipid biology and hepatocyte physiology. Lipid droplets have often been viewed merely as inert fat repositories, yet this research vividly illustrates their complex regulation and critical contribution to cellular health. It also highlights the liver’s remarkable capacity for protein quality control and adaptation—a capacity compromised by external toxins such as alcohol, with profound pathological consequences.
Additional relevance emerges from the study’s contribution to predictive medicine. Understanding how the VCP-HSD17β13 axis operates enables clinicians to potentially identify patients whose cellular systems are compromised, rendering them more susceptible to alcohol’s deleterious effects. This paves the way for personalized risk assessments and preemptive interventions, consistent with Mayo Clinic’s larger Precure initiative, which aims to intercept disease progression through early molecular detection and targeted therapeutics.
The rigorous investigation, published in the Journal of Cell Biology, exemplifies modern molecular biology’s power to unravel the interplay between lifestyle factors and cellular machinery. It also accentuates the importance of interdisciplinary research bridging biochemistry, cell biology, and clinical medicine to confront pervasive health challenges like fatty liver disease. As alcohol consumption remains widespread globally, these mechanistic insights are critical for public health strategies seeking to mitigate chronic liver conditions.
In conclusion, the elucidation of ethanol’s disruption of VCP-mediated protein recycling introduces a vital piece to the puzzle of fatty liver pathogenesis. By linking alcohol abuse directly to the malfunction of hepatocellular protein quality control systems, this study offers a clarion call for intensified research into molecular therapies. The seamless convergence of cutting-edge cell biology techniques and clinical insight promises not only enhanced disease comprehension but also innovative pathways towards effective prevention and treatment.
Subject of Research: Mechanistic insights into alcoholic fatty liver disease via disruption of VCP-mediated lipid droplet protein recycling.
Article Title: An ethanol-induced loss of the lipid droplet–associated segregase VCP/p97 leads to hepatic steatosis
News Publication Date: 29-Jul-2025
Web References:
https://rupress.org/jcb/article/224/8/e202408205/278160/An-ethanol-induced-loss-of-the-lipid-droplet
https://rupress.org/jcb/article/224/8/e202506103/278158/New-insights-into-lipid-droplet-breakdown-in?searchresult=1
References:
Detailed within the original Journal of Cell Biology publication.
Keywords: fatty liver disease, alcoholic liver disease, valosin-containing protein, VCP, lipid droplets, HSD17β13, ethanol toxicity, hepatocyte biology, protein recycling, lysosome, metabolic dysfunction, hepatic steatosis
Tags: alcohol-related liver damagebiochemical processes in hepatocytesconnection between alcohol and liver diseaseexcessive alcohol consumptionfatty liver diseasehepatic steatosis mechanismsliver function impairmentliver health and alcoholmetabolic dysfunction-associated steatotic liver diseasemetabolic stress and liver healthprotein recycling in liver cellsvalosin-containing protein role