Breaking Through Chemotherapy Resistance: Targeting p300 Unveils a Novel Cellular Vulnerability in Cancer Treatment
In the relentless battle against cancer, one of the most formidable obstacles is the ability of tumors to develop resistance against chemotherapy drugs. These chemoresistant cancer cells manage to circumvent the lethal effects of treatment by adapting their biological machinery, rendering conventional therapies increasingly ineffective. However, a groundbreaking study conducted by researchers at the Sylvester Comprehensive Cancer Center, part of the University of Miami Miller School of Medicine, introduces a transformative approach that re-sensitizes resistant tumors by exploiting a novel stress response triggered within cancer cells.
Central to this discovery is the protein p300, a multifunctional epigenetic regulator known for its role in controlling transcription – the process by which DNA instructions guide protein synthesis. Under normal circumstances, when cellular DNA is damaged—by environmental factors, ultraviolet light, or chemotherapy agents—the cell employs an essential safeguard: it pauses transcription. This halt is akin to an emergency stop in a complex assembly line, preventing the production of faulty proteins that could jeopardize cellular integrity. p300 acts as a molecular traffic officer, orchestrating the clearance and resolution of stalled transcription complexes and ensuring the smooth resumption of gene expression once damage is repaired.
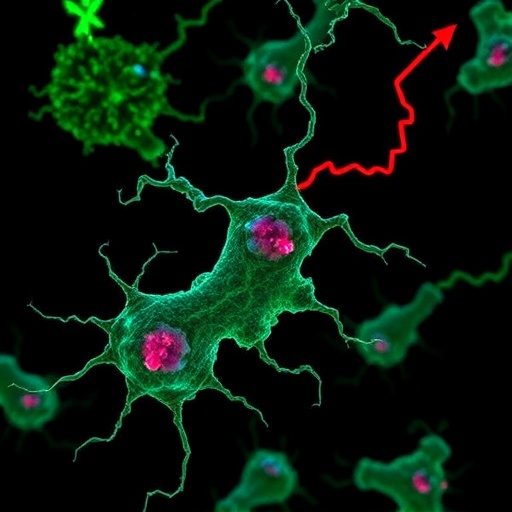
Yet, in chemo-resistant cancer cells, this regulatory mechanism is subverted. Instead of halting to fix DNA lesions, these malignant cells press forward, relentlessly transcribing damaged DNA and producing a surge of defective proteins. The innovative findings from Sylvester’s team reveal that inhibiting p300 dismantles its “traffic control” function, causing transcription machinery to accumulate at DNA lesions. This unchecked transcription despite DNA damage induces a unique and intense intracellular stress state, far beyond conventional genotoxic effects.
This cascades into a proteotoxic nightmare within the cancer cell. The damaged DNA template churns out unstable, misfolded proteins that clog the endoplasmic reticulum (ER)—the cell’s protein-folding factory. The ER’s quality control, known as the unfolded protein response (UPR), is overwhelmed, sending distress signals that resemble an engine overheating from overexertion. Crucially, this novel form of cellular stress becomes a therapeutic Achilles’ heel for tumors that had previously mastered DNA damage tolerance.
Experimentally, the researchers demonstrated that platinum-based chemotherapy, which traditionally forms the backbone of cancer treatment, has limited efficacy against resistant tumors by itself. Similarly, inhibiting p300 alone did not dramatically reduce tumor growth. However, the combination of p300 blockade with platinum chemotherapy generated a striking synergistic effect. This duo selectively obliterated tumor cells by overloading them with a lethal onslaught of unresolved protein damage and unresolved transcriptional activity.
Physiologically, this approach capitalizes on “forcing” cancer cells to transcribe through damaged DNA, which they usually avoid, thereby escalating internal stress to fatal levels. Ramiro Verdun, Ph.D., a leading researcher on the study, likened it to overloading a faulty electrical circuit: it’s not the quantity of damage that is increased, but the cell’s inability to manage the damage that proves fatal. This revolutionary concept reframes the long-held narrative around chemotherapy resistance, shifting focus from overwhelming tumors with more DNA damage to instead manipulating their stress responses.
Clinically, this insight holds tremendous promise. Platinum chemotherapies are often limited by toxicity to vital organs such as kidneys and the nervous system, constraining treatment dosages. The novel strategy circumvents this by increasing tumor vulnerability to existing chemotherapy doses, rather than escalating drug intensity. This could significantly enhance therapeutic outcomes while minimizing adverse side effects. In patient-derived xenograft models representing colorectal cancer and pediatric osteosarcoma—both notoriously difficult to treat—the dual therapy markedly shrank tumors and extended survival, signaling a major leap forward in precision oncology.
Ramin Shiekhattar, Ph.D., co-leader of the Cancer Epigenetics Program at Sylvester, emphasized the broader implications. With this newfound understanding of transcriptional stress induced by DNA damage bypass, researchers can now design smarter, anticipatory combination therapies. Rather than reacting to resistance, this strategy predicts and preempts tumor adaptations, potentially prolonging the efficacy of standard chemotherapeutic regimens and benefiting a wider patient population.
At the molecular level, this study uniquely elucidates the interplay between DNA repair pathways and transcription dynamics orchestrated by p300. It showcases how the failure to pause and rectify transcription in damaged DNA results in an unresolved “traffic jam” within gene expression pathways, culminating in ER stress and proteostasis collapse. By pinpointing p300 as a pivotal molecular node, the research opens new avenues for targeting epigenetic regulators in drug-resistant cancers.
Furthermore, the approach holds distinct value in its ability to re-sensitize tumors without adding chemotherapy-associated toxic burden—a significant advantage considering the delicate balance oncologists face in dosing. Lluis Morey, Ph.D., a co-author, remarked that this research doesn’t merely add incremental knowledge to the DNA repair field; it fundamentally reframes the problem by demonstrating that the critical danger lies not only in DNA damage itself, but in the cellular consequences of failing to properly respond to that damage.
From a translational perspective, this work is a clarion call to revisit and revamp current cancer treatment paradigms. By integrating epigenetic inhibition targeting p300 with conventional chemotherapies, it presents a dual-front assault on chemoresistant cancers. Such strategies could catalyze the development of combination therapies that are both more effective and better tolerated, particularly for patients who previously had few or no treatment options.
This study, published in the esteemed journal Genes & Development, underscores the power of deciphering fundamental cellular stress mechanisms to achieve clinical breakthroughs. It sets the stage for future clinical trials that could validate p300 inhibitors as an adjunct to chemotherapy, heralding a new era where overcoming drug resistance becomes a realistic goal rather than an elusive challenge.
As research progresses, the discovery offers hope for millions battling chemo-refractory cancers worldwide. By exploiting the vulnerability of cancer cells that refuse to “hit pause,” scientists are charting an innovative pathway toward more durable, targeted, and effective cancer therapies that could transform patient lives in profound ways.
Subject of Research: Chemotherapy resistance in cancer cells, transcriptional regulation by p300, and exploitation of proteotoxic stress for cancer therapy.
Article Title: “Bypass of blocking lesions by RNAPII reveals a novel stress induced by DNA damage”
News Publication Date: February 5, 2026
Web References:
Sylvester Comprehensive Cancer Center: https://umiamihealth.org/en/sylvester-comprehensive-cancer-center
Original study in Genes & Development: https://genesdev.cshlp.org/content/early/2026/02/04/gad.353164.125.abstract
Sylvester Cancer on X: https://x.com/SylvesterCancer
References: Funding and disclosures available within the original publication.
Keywords: Cancer treatments, Chemotherapy, Cancer cells, Epigenomics, Epigenetic markers, Molecular genetics, Genomics, DNA repair
Tags: cellular vulnerability in cancer therapychemotherapy and tumor adaptationchemotherapy resistance in cancerepigenetic regulation in cancer treatmentnovel stress response in cancer cellsovercoming drug resistance in tumorsprotein synthesis and cancer cellsre-sensitizing tumors to chemotherapyrole of p300 protein in cancerSylvester Comprehensive Cancer Center researchtargeted cancer treatment strategiestranscription control in cancer