Credit: Vanderbilt University
WASHINGTON — Researchers have developed the first sensor capable of objectively identifying inflammatory bowel disease (IBD) and distinguishing between its two subtypes. The device represents a substantial achievement toward a more personalized approach to diagnosing and treating IBD, a chronic inflammation of the gastrointestinal tract affecting more than 1 million Americans.
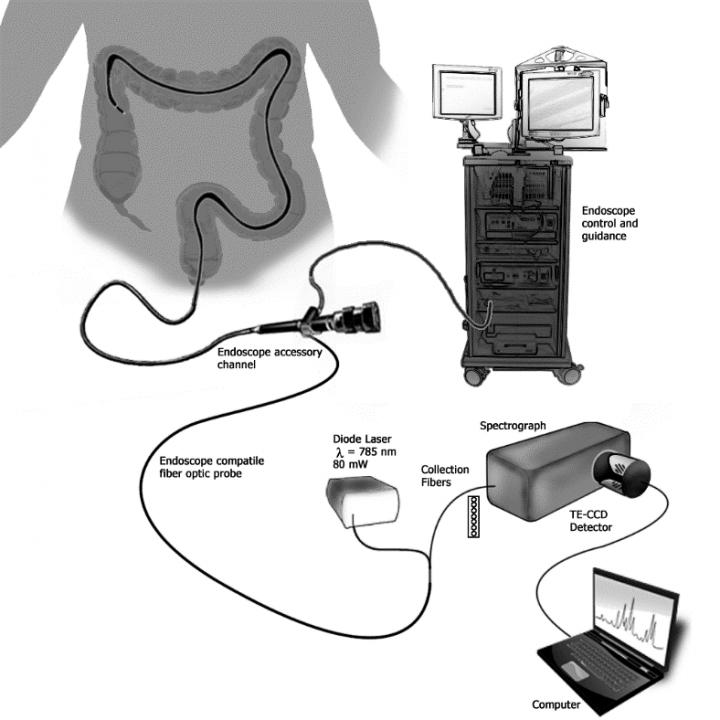
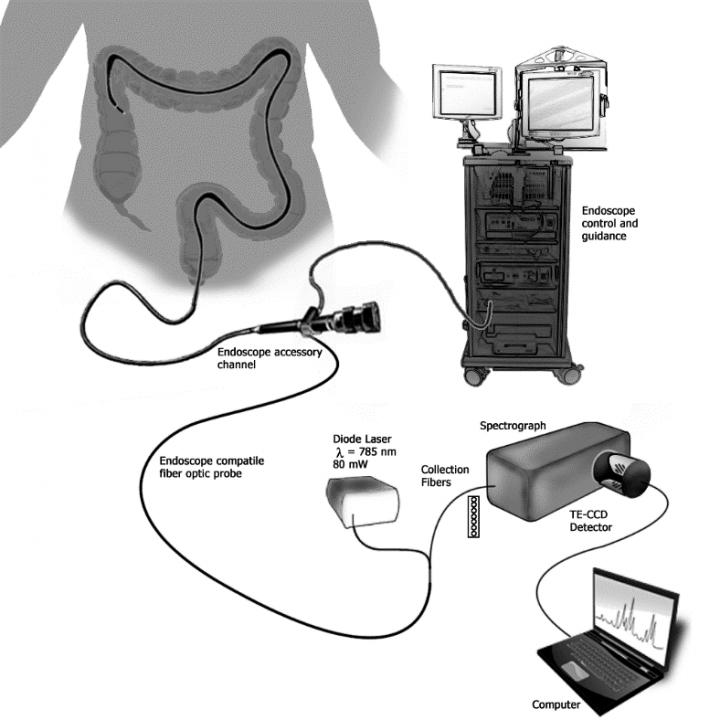
Current diagnostic and treatment procedures for IBD are inexact and rely largely on trial-and-error. In The Optical Society's journal Biomedical Optics Express, researchers report on a pilot study of a custom-developed endoscope that uses the chemical-fingerprinting technique Raman spectroscopy to detect molecular markers of IBD in the colon.
The sensor is designed as a minimally-invasive probe that can be easily integrated into a routine colonoscopy exam. After further refining, the researchers say doctors could use the device to help diagnose IBD and evaluate a patient's response to treatment.
"With current methods, ultimately the diagnosis is dependent on how the patient responds to therapy over time, and you often don't know the diagnosis until it's been a few years," said Anita Mahadevan-Jansen of Vanderbilt University, USA, senior author of the paper, who initiated the project after a personal experience with IBD. "That's why we decided to use a light-based method to probe the biochemistry of what's going on in the colon. Our goal is to use Raman spectroscopy to look at the actual inflammatory signals."
Seeking a gold standard for diagnosis
IBD occurs in two subtypes: ulcerative colitis (UC), which is typically confined to the colon, and Crohn's disease, which can occur in any part of the gastrointestinal tract. They can cause similar symptoms such as severe diarrhea, pain, fatigue and weight loss, yet the two types respond differently to available treatments, which include drugs, dietary interventions and surgery.
Doctors currently use a combination of clinical, radiologic and pathological methods to diagnose a patient's IBD subtype and guide treatment decisions, but these methods detect symptoms, rather than the underlying source of disease, and the process has lacked an objective gold standard. As a result, up to 15 percent of patients are diagnosed with indeterminate colitis, meaning the subtype is unknown, and an additional 5 to 14 percent have their IBD reclassified based on how they respond to treatment.
Previous research conducted in tissue samples from people with IBD showed that UC and Crohn's disease have different molecular signatures. The new probe detects these signatures in order to glean information about not only disease subtype, but also the current degree of inflammation and even early indicators of IBD that occur before observable changes in the intestinal tissue.
"Most people go through baseline colonoscopy as part of routine care, and you could imagine using this to get a baseline Raman signal for each person," said Mahadevan-Jansen. "If someone presents with IBD symptoms later on, you can use our system again to determine if it's more likely to be UC or Crohn's. Then once they are being treated, you have an objective measure to track their response because you can use the device to actually quantify mild, moderate or severe inflammation."
Creating a clinic-ready device
To develop the probe, the researchers first used tissue samples and animal models to identify preliminary biomarkers and spectral signatures consistent with IBD. They then custom-built a portable Raman spectroscopy system with a 785 nm diode laser and fiber-optic probe that delivers 80 mW to the surface of the colon.
"The customization was both the packaging – to make sure it can fit easily in the endoscopy channel and bend through the turns of the colon – and to probe the right depth in the tissues we are looking at to make sure we can get a robust measurement," explained Mahadevan-Jansen.
Raman spectroscopy has been previously applied in the gastrointestinal tract for cancer detection, but using it to measure markers of inflammation poses some unique challenges because the signals are far more subtle. This necessitated special engineering, for example, to include filters that eliminate the Raman signature produced by the components of the probe itself.
In their pilot test, the researchers used the device in 15 patients with an existing diagnosis of Crohn's disease, eight patients with UC and eight healthy volunteers. In general, the results suggest high sensitivity (the ability to detect IBD) but poor specificity (the ability to differentiate between subtypes), though results vary depending on the degree of inflammation and where the measurement was taken. When measuring the right colon in patients with active inflammation, for example, the device detected Crohn's disease with a sensitivity of 90 percent and a specificity of 75, compared to 86 percent and 39 percent, respectively, when results are averaged across all disease states, inflammation levels and locations within the colon.
Looking ahead
The researchers are now focused on refining a set of algorithms that help doctors interpret test results for a given patient. To improve the test's specificity, the team is analyzing data from an expanded cohort of patients to discern how factors such as gender, diet, demographics and treatment regimen influence the Raman signature. Ultimately, they envision a system that combines key information about the patient with Raman spectra to deliver, in a matter of seconds, tailored results that can inform a diagnosis or help track a patient's response to treatment.
"It's a unique way of thinking about personalized medicine that takes into account all sorts of information – beyond just the genome – including demographics and many other factors that make a person unique," said Mahadevan-Jansen. "Our lab has really pushed to find ways to apply optical technology to support this kind of personalized medicine."
The researchers are also pursuing studies in animal models to further understand the sources of various molecular signals, identify the types of changes that can be expected as a result of treatment and determine whether the device could be used to detect IBD or risk factors at even earlier stages.
###
Paper: I. Pence, D. Beaulieu, S. Horst, X. Bi, A. Herline, D. Schwartz, A. Mahevan-Jansen, "Clinical characterization of in vivo inflammatory bowel disease with Raman spectroscopy," Biomedical Optics Express, Vol. 8, Issue 2, 524-535, (2017).
DOI: 10.1364/BOE.8.000524
About Biomedical Optics Express
Biomedical Optics Express is OSA's principal outlet for serving the biomedical optics community with rapid, open-access, peer-reviewed papers related to optics, photonics and imaging in the life sciences. The journal scope encompasses theoretical modeling and simulations, technology development, and biomedical studies and clinical applications. It is published by The Optical Society and edited by Christoph Hitzenberger, Medical University of Vienna. Biomedical Optics Express is an open-access journal and is available at no cost to readers online at: OSA Publishing.
About The Optical Society
Founded in 1916, The Optical Society (OSA) is the leading professional organization for scientists, engineers, students and business leaders who fuel discoveries, shape real-life applications and accelerate achievements in the science of light. Through world-renowned publications, meetings and membership initiatives, OSA provides quality research, inspired interactions and dedicated resources for its extensive global network of optics and photonics experts. For more information, visit osa.org/100.
Media Contacts:
Rebecca B. Andersen
The Optical Society
[email protected]
+1 202.416.1443
Joshua Miller
The Optical Society
[email protected]
+1 202.416.1435
Media Contact
Joshua Miller
[email protected]
202-416-1435
@opticalsociety
http://www.osa.org
############
Story Source: Materials provided by Scienmag