A revolutionary nebuliser developed by RMIT University in researchers in Melbourne, could one day deliver life-saving cancer drugs and vaccines traditionally given by injection.
Cheap, light-weight and portable, the advanced nebuliser delivers precise drug doses to patients with life-threatening or debilitating lung conditions including cancer, tuberculosis, asthma and cystic fibrosis.
But the Respite™ nebuliser also has the potential to be used to administer insulin to people with diabetes or to painlessly vaccinate infants currently subjected to needles.
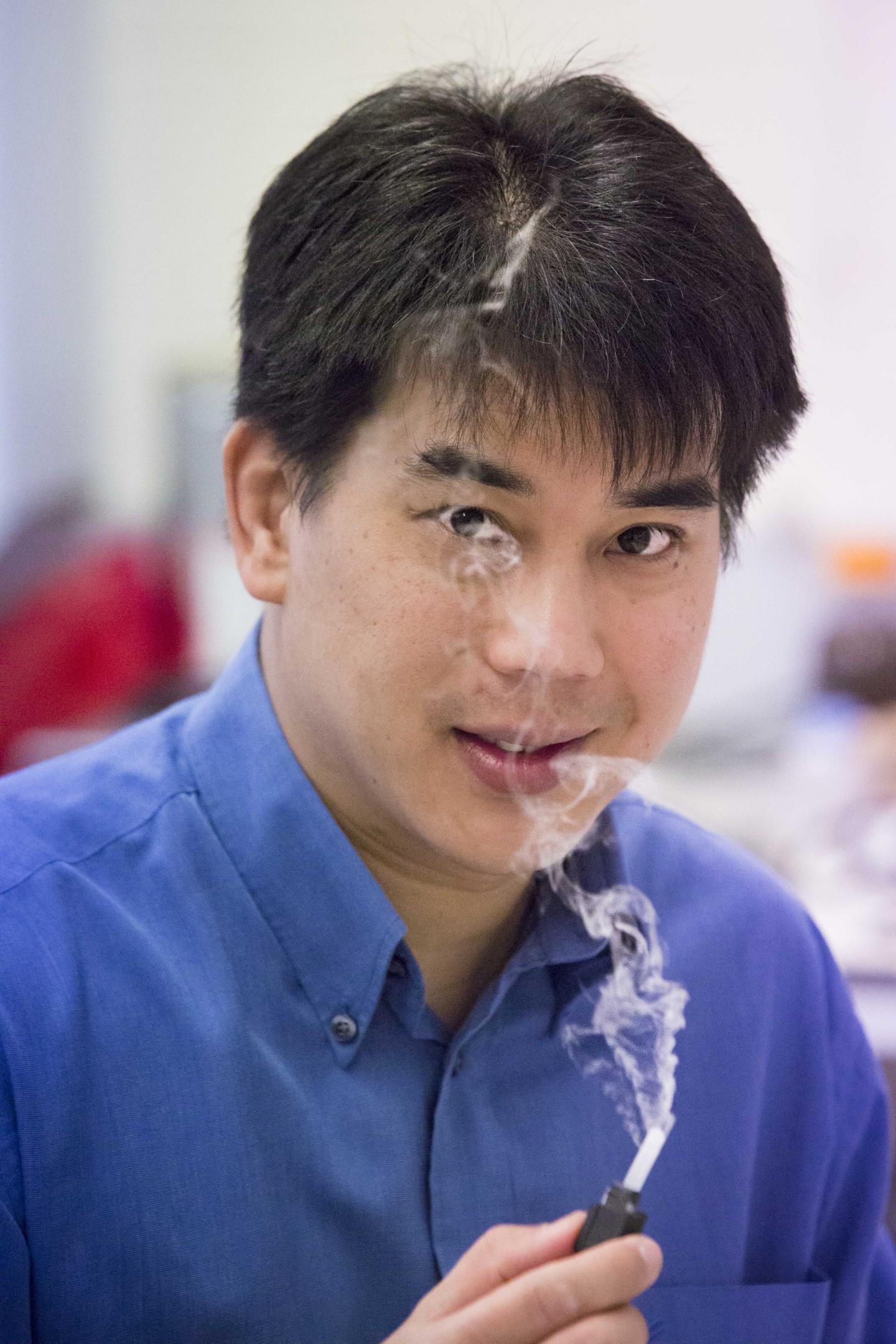
Professor Leslie Yeo, Director of RMIT's MicroNanophysics Research Laboratory, said the Respite technology had the potential to revolutionise how patients were treated with drugs, including people with lung cancer whose poor survival rates have stayed stable despite significant therapeutic advances in recent years.
"Anything we can nebulise, we can potentially deliver," Yeo said.
"The problem with normal puffers is that only 30 per cent of the drugs actually get to the lungs, the rest is lost in the mouth – which isn't a problem if the drugs are cheap but is when they are expensive.
"The most important aspect of our device is that it does not require inhalation to generate the aerosols as with the ubiquitous inhalers, which can be a problem for people already suffering compromised lung function."
Yeo said traditional inhalers also require hand-breath coordination to use and elderly and very young patients must be taught to avoid misusing.
"And unlike one-size-fits-all inhalers, Respite allows the dose to be adjusted based on a patient's size, age, gender, physiological profile and disease severity."
The design does not require meshes or nozzles unlike other nebulisers, so there is no clogging or fouling problems that diminish performance.
The Respite technology uses sound waves to excite the surface of the fluid or drug. This generates a fine mist capable of delivering much larger molecules directly to the lungs.
Rigorous lab tests have proved the device capable of delivering next generation drugs such as proteins, peptides and DNA to the lungs without a patient having to inhale.
The device delivers drugs at rates of up to 3 ml/min, compared to the much smaller doses of 0.4 ml/min benchmark of current nebulisers.
Recent trials in Melbourne also showed sheep given a DNA flu vaccine via a nebuliser had comparable immune responses to animals injected with the vaccine.
A Professor of Chemical Engineering and an Australian Research Council Future Fellow, Yeo believes the device has enormous potential, particularly for people with lung cancer.
"The five-year survival rate for lung cancer remains around 15 per cent despite the significant therapeutic advances achieved in recent years and currently, there are no personalised delivery devices for inhaled cancer drugs to improve these clinical outcomes," he said.
"Our nebuliser addresses this gap as a low-cost and convenient yet efficient method of delivering oncolytics directly to the lungs, potentially revolutionising the treatment of lung cancer."
Lung cancer is the leading cause of deaths by cancer and the fifth most commonly diagnosed cancer in Australia.
The nebuliser can also be used for a range of non-pharmaceutical applications such as perfumes, cosmetics and sterilisation of equipment and surfaces.
###





