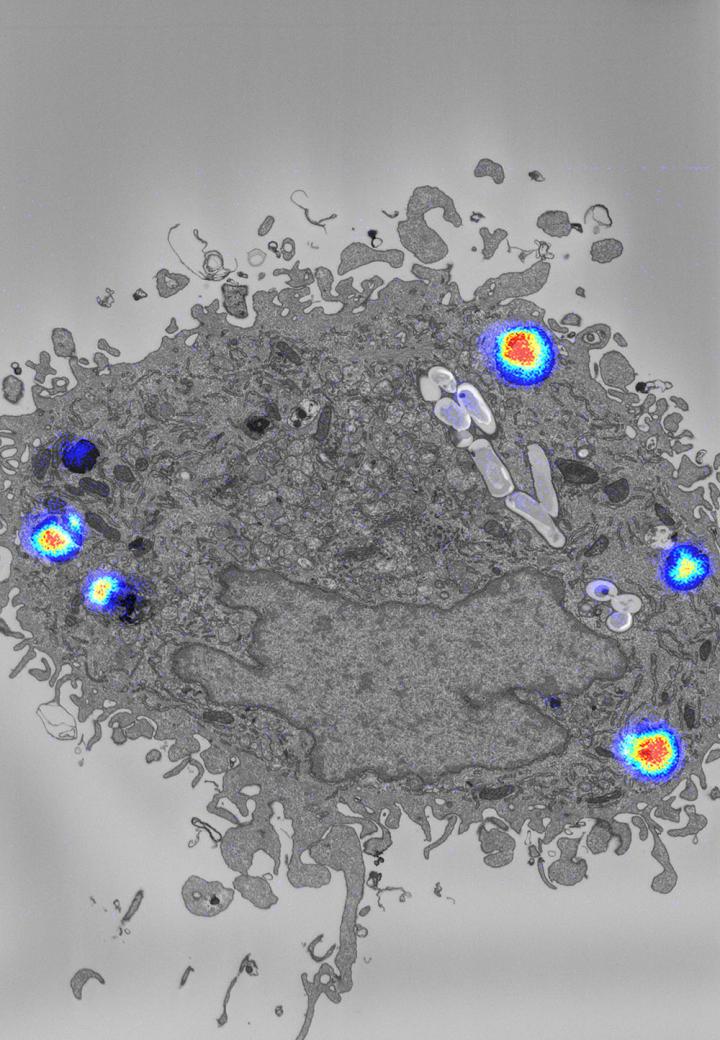
Credit: Daniel Greenwood, Francis Crick Institute.
Scientists have developed a new technique that enables them to visualise how well antibiotics against tuberculosis (TB) reach their pathogenic targets inside human hosts. The findings, published in the journal Science, boost our understanding of how antibiotics work and could help guide the development of new antibiotics, which are much-needed in the battle against drug-resistance.
The Crick-led team used the technique to observe the TB drug, bedaquiline, in action in human cells infected with the TB-causing bacterium, Mycobacterium tuberculosis (Mtb). They found that bedaquiline accumulates in lipid droplets inside the host cells, forming a reservoir that supplies the drug to Mtb over time. The work was done in collaboration with scientists at GlaxoSmithKline and the University of Western Australia.
“Bedaquiline is the first newly approved antibiotic for TB treatment in 50 years, but until now, we didn’t understand how a compound that doesn’t dissolve in water could be so effective in treating TB,” explains Daniel Greenwood, Crick PhD student and first author of the paper.
“Normally, compounds that only dissolve in lipids, known as lipophilic compounds, are often abandoned during drug development because they tend to bind to proteins and fats in our bodies in a non-specific way. We wondered how such a drug could ever reach the bacteria. Our surprising findings show that even very lipophilic antibiotics like bedaquiline are worth pursuing in drug development. In the case of TB, this conventionally undesirable trait actually boosts drug delivery.”
TB treatment
TB remains one of the world’s deadliest infectious diseases, with over a million TB-related deaths worldwide each year.
When a person is infected with Mtb, their immune system tries to clear the pathogen by calling upon specialised immune cells called macrophages that recognise and engulf Mtb. But the bacteria often find ways to survive and reproduce, causing disease. Patients require a minimum of four antibiotics for at least six months to overcome the infection.
It was previously unknown whether antibiotics penetrate into all the compartments of the macrophage where the Mtb hide and replicate.
The method pioneered in this study, which combines three types of imaging (correlated light, electron and nano-scale ion microscopy), allows researchers to visualise the distribution of TB drugs in Mtb-infected human macrophages at high resolution, for the first time.
A test-case TB drug
Using bedaquiline as a test-case, they infected human macrophages with Mtb, and after two days, treated them with the drug. Their imaging results revealed that bedaquiline accumulated in numerous compartments of the cell, most notably, inside lipid droplets.
The bacteria can interact with and consume these lipid droplets. However, the team didn’t know if bedaquiline would be transferred to the bacteria, or whether the lipid droplets were absorbing the antibiotic and preventing it from reaching the bacteria. Adding a chemical that prevented lipid droplets from forming significantly reduced the amount of bedaquiline in Mtb, suggesting that the lipid droplets are responsible for transferring antibiotic to the bacteria.
“Now that we can see exactly where antibiotics go once they enter macrophages, we can build up a much clearer picture of how they reach their targets, and harness these observations to design more effective treatments in the future, not only for TB but for other infectious diseases too,” says Max Gutierrez, Crick group leader and senior author of the paper.
###
Media Contact
Greta Keenan
[email protected]




