Obstructive sleep apnea and short sleep duration have distinct clinical impacts; clinicians should avoid a ‘one-size-fits-all’ approach through proper diagnosis to prevent and treat sleep disorders, according to a new study in the journal CHEST®
Credit: CHEST
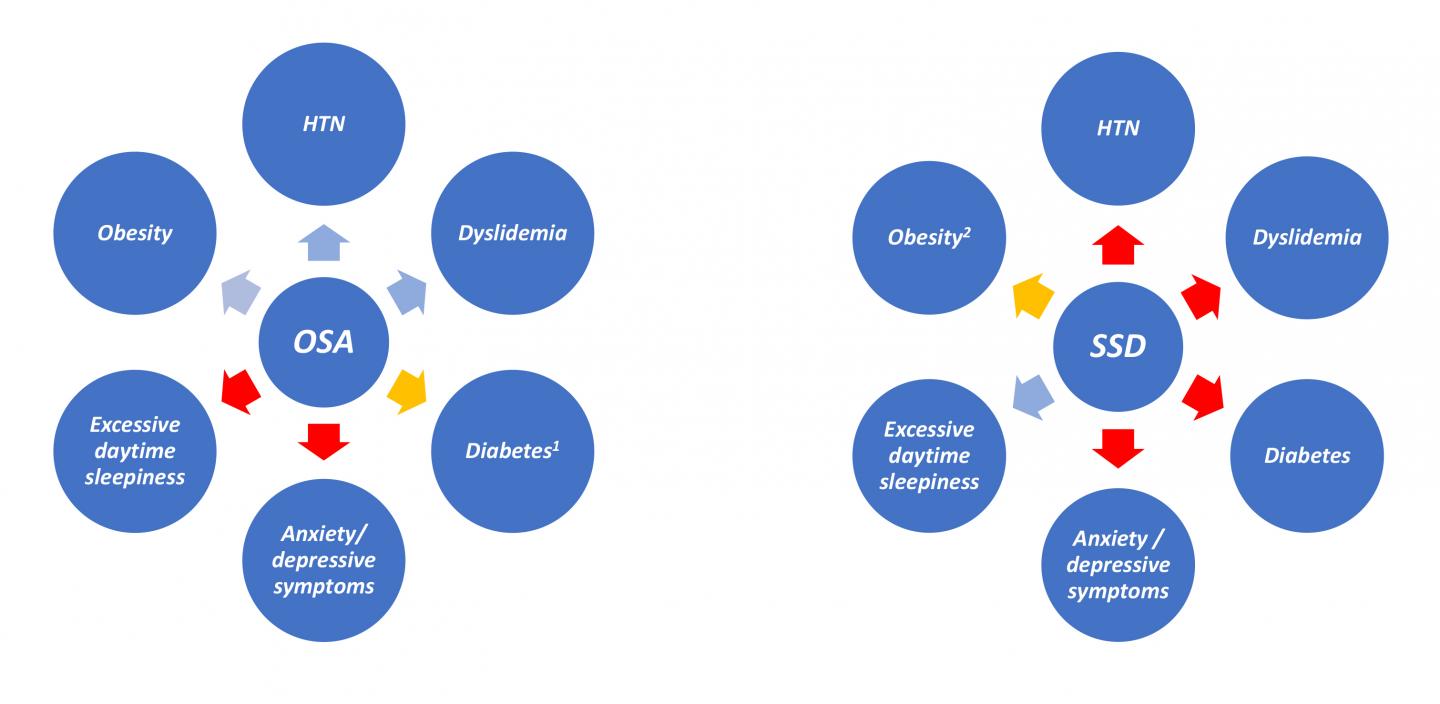
Glenview, IL, April 1, 2019 – A new study appearing in the journal CHEST®, published by Elsevier, may change the way we think about sleep disorders. In this study led by Dr. Luciano F. Drager, obstructive sleep apnea (OSA) and short sleep duration (SSD) were compared with excessive daytime sleepiness; anxiety/depressive symptoms; and several cardiometabolic risk factors including obesity, hypertension, diabetes and dyslipidemia. Using a large sample of adults, investigators found that SSD, but not OSA, was independently associated with daytime sleepiness. In contrast, OSA, but not SSD, was independently associated with obesity, hypertension, and dyslipidemia. Neither was independently associated with anxiety or depression.
Tracking OSA and SSD in the same investigation allowed researchers to compare the potential consequences of the two most common sleep disorders, and the results of this study challenge some traditional beliefs. “Our findings suggest potential distinct clinical impacts of OSA and SSD,” explained Luciano F. Drager, MD, PhD, of the Center of Clinical and Epidemiologic Research (CPCE); Hypertension Unit, Heart Institute (InCor); and Hypertension Unit, Renal Division, of the University of Sao Paulo, Sao Paulo, Brazil. “The potential impact on patient care is that our results underscore the need to advance our knowledge of OSA and SSD determination to avoid the ‘one-size-fits-all’ approach and instead tailor personalized preventive, diagnostic, prognostic, and therapeutic strategies to our patients.”
Data came from close to 2,100 participants from the cross-sectional Brazilian Longitudinal Study of Adult Health (ELSA-Brasil), a long-term study of Brazilian civil servants (ages 35 to 74 years) that aims to help investigators learn about the development and progression of clinical and subclinical chronic diseases. Participants were not referred for sleep studies and anyone being treated for OSA, receiving sleep-interfering medications, or engaged in nocturnal or shift work was excluded.
More sleep disorders were identified in patients studied than anticipated, including almost one third with OSA. More than one quarter of participants had SSD, meaning that they slept on average less than six hours a night. A significant overlap of about 11 percent of the patients manifested both OSA and SSD, although no interaction was found between OSA and SSD.
The study reported some findings that are contrary to traditional thinking. For instance, because this study measured sleep duration objectively with a device (wrist actigraphy over a seven-day period), rather than relying on patient self-reporting, the investigators found more people with inappropriate sleep durations than commonly thought. “In this study, only one quarter of participants slept seven to eight hours on average, the most highly recommended sleep duration for middle-aged adults,” said Dr. Drager. While individuals with SSD were more likely to report excessive sleepiness during the daytime, SSD was not associated with obesity, hypertension, or dyslipidemia.
Another surprising finding was that OSA was not associated with excessive daytime sleepiness, even if OSA was severe. However, OSA was, associated with obesity, hypertension, and dyslipidemia, but not with anxiety or depression. In subgroup analysis, obesity was associated with all levels of OSA severity, but only severe OSA was associated with hypertension. “Our findings do not mean that OSA never causes sleepiness, but in clinical practice a significant proportion of patients with OSA are asymptomatic or minimally symptomatic,” noted Dr. Drager.
Dr. Drager suggests that in previous studies any positive associations found between SSD and cardiometabolic risk factors could have been due to “occult” (non-apparent) OSA. “The additional lack of association of SSD with obesity, dyslipidemia, and diabetes in our large cohort reinforces the potential need to reappraise the evidence on subjective SSD and cardiometabolic risk factors,” commented Dr. Drager.
###
Media Contact
Andrea Camino
[email protected]
Related Journal Article
http://dx.




