How do neurological disorders arise that are caused, triggered, or influenced by antibodies? What better possibilities are there for diagnosis – and above all for treatment? These are the questions addressed by the new Clinical Research Unit “BecauseY” headed by Charité – Universitätsmedizin Berlin. Innovative treatment options will especially benefit patients who at first glance are not suspected of having an antibody-mediated neurological disease. The German Research Foundation (DFG) is funding the collaborative project with 6.2 million euros for an initial term of four years.
Neuroinflammatory disorders can be caused by pathogens such as viruses, bacteria, and fungi or by autoimmune processes that damage the body’s own brain or nerve tissue. In many patients, “neuronal autoantibodies” can impair communication between neurons, triggering autoimmune disorders of the nervous system. The idea that antibodies can cause diseases such as dementia, epilepsy, psychosis, and a severe form of encephalitis called autoimmune encephalitis is a relatively recent discovery that has reshaped the face of neurology and psychiatry.
“Current research suggests that many other neurological and psychiatric symptoms are associated with misdirected immune processes, or autoimmunity. Autoantibodies can also have disease-modifying effects in a number of conditions,” explains Prof. Matthias Endres, Director of the Department of Neurology with Experimental Neurology at Charité and the spokesperson for the Clinical Research Unit. “The need for research in this area is enormous. That’s why the goal of the new alliance is to study the emergence and disease mechanisms of antibody-mediated neurological diseases in more detail and to gain a better understanding of them.”
Center for understanding and treating antibody-mediated neurological diseases
To this end, the Clinical Research Unit will determine the prevalence, targets, and functions of autoantibodies in neurological disease and develop new diagnostic tests and brain imaging techniques as well as innovative therapies. The unit will be structured around a center where researchers working in basic research and those focused on clinical questions work hand-in-hand both on-site at the Department of Neurology and at various laboratories of project partners. Samples taken from patients, such as blood or cerebrospinal fluid, will feed directly into research, while laboratory findings are also incorporated into treatment studies.
“This is the first center of its kind explicitly focused on antibody-mediated disease,” says Prof. Harald Prüss, who also works at the Department of Neurology with Experimental Neurology and is the coordinator of the Clinical Research Unit. He continues, “This is where we come in with BecauseY. We will not only be following and supporting patients holistically throughout the course of their disease with a personalized approach, but we will also replicating the underlying autoantibodies to understand how they work while applying new therapies. This interface between experimental and clinical research will mean our findings will benefit patients directly.” Additionally, the researchers believe that certain autoantibodies also play a role in diseases and conditions not previously associated with autoimmunity, such as stroke, neurodegenerative forms of dementia, and developmental disorders. Completely new therapeutic approaches are also expected from this research.
About the BecauseY Clinical Research Unit
The BecauseY Clinical Research Unit at Charité and the German Center for Neurodegenerative Diseases (DZNE) does research on antibody-mediated neurological diseases. The unit gets its name from the Y-shaped structure characteristic of antibodies. There will be eight subprojects, all dealing with the intersection between autoimmunity and neuroscience and clustered within three thematic areas of emphasis: understanding mechanisms of disease, diagnosis, and next-generation selective immune therapies. The researchers will stay in continuous dialogue, especially about fundamental findings relating to disease mechanisms, biobank samples, clinical data, new diagnostic methods, and initial applications of innovative immune therapies. The German Research Foundation (DFG) typically supports Clinical Research Units (CRUs) for up to eight years, divided into two four-year funding periods.
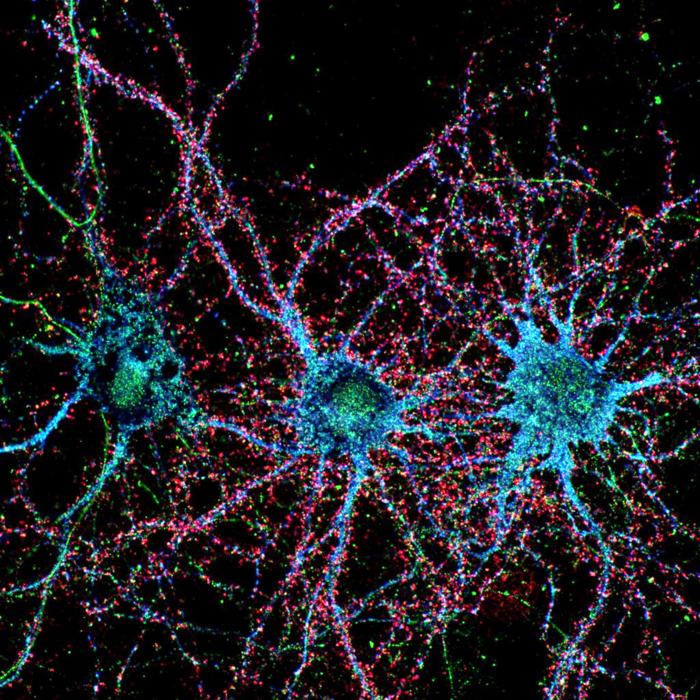
Credit: Isabel Bünger
How do neurological disorders arise that are caused, triggered, or influenced by antibodies? What better possibilities are there for diagnosis – and above all for treatment? These are the questions addressed by the new Clinical Research Unit “BecauseY” headed by Charité – Universitätsmedizin Berlin. Innovative treatment options will especially benefit patients who at first glance are not suspected of having an antibody-mediated neurological disease. The German Research Foundation (DFG) is funding the collaborative project with 6.2 million euros for an initial term of four years.
Neuroinflammatory disorders can be caused by pathogens such as viruses, bacteria, and fungi or by autoimmune processes that damage the body’s own brain or nerve tissue. In many patients, “neuronal autoantibodies” can impair communication between neurons, triggering autoimmune disorders of the nervous system. The idea that antibodies can cause diseases such as dementia, epilepsy, psychosis, and a severe form of encephalitis called autoimmune encephalitis is a relatively recent discovery that has reshaped the face of neurology and psychiatry.
“Current research suggests that many other neurological and psychiatric symptoms are associated with misdirected immune processes, or autoimmunity. Autoantibodies can also have disease-modifying effects in a number of conditions,” explains Prof. Matthias Endres, Director of the Department of Neurology with Experimental Neurology at Charité and the spokesperson for the Clinical Research Unit. “The need for research in this area is enormous. That’s why the goal of the new alliance is to study the emergence and disease mechanisms of antibody-mediated neurological diseases in more detail and to gain a better understanding of them.”
Center for understanding and treating antibody-mediated neurological diseases
To this end, the Clinical Research Unit will determine the prevalence, targets, and functions of autoantibodies in neurological disease and develop new diagnostic tests and brain imaging techniques as well as innovative therapies. The unit will be structured around a center where researchers working in basic research and those focused on clinical questions work hand-in-hand both on-site at the Department of Neurology and at various laboratories of project partners. Samples taken from patients, such as blood or cerebrospinal fluid, will feed directly into research, while laboratory findings are also incorporated into treatment studies.
“This is the first center of its kind explicitly focused on antibody-mediated disease,” says Prof. Harald Prüss, who also works at the Department of Neurology with Experimental Neurology and is the coordinator of the Clinical Research Unit. He continues, “This is where we come in with BecauseY. We will not only be following and supporting patients holistically throughout the course of their disease with a personalized approach, but we will also replicating the underlying autoantibodies to understand how they work while applying new therapies. This interface between experimental and clinical research will mean our findings will benefit patients directly.” Additionally, the researchers believe that certain autoantibodies also play a role in diseases and conditions not previously associated with autoimmunity, such as stroke, neurodegenerative forms of dementia, and developmental disorders. Completely new therapeutic approaches are also expected from this research.
About the BecauseY Clinical Research Unit
The BecauseY Clinical Research Unit at Charité and the German Center for Neurodegenerative Diseases (DZNE) does research on antibody-mediated neurological diseases. The unit gets its name from the Y-shaped structure characteristic of antibodies. There will be eight subprojects, all dealing with the intersection between autoimmunity and neuroscience and clustered within three thematic areas of emphasis: understanding mechanisms of disease, diagnosis, and next-generation selective immune therapies. The researchers will stay in continuous dialogue, especially about fundamental findings relating to disease mechanisms, biobank samples, clinical data, new diagnostic methods, and initial applications of innovative immune therapies. The German Research Foundation (DFG) typically supports Clinical Research Units (CRUs) for up to eight years, divided into two four-year funding periods.



