Encephalocraniocutaneous lipomatosis (ECL) is a rare neurocutaneous disorder characterized by the presence of lipomas affecting the brain, craniofacial region, and skin. The condition often manifests early in life, with symptoms that can vary widely among patients. Recent advancements in neuroradiological techniques have shed new light on this complex disorder, aiding in both diagnosis and treatment planning. This exploration into ECL provides a deeper understanding of its neuroanatomical implications, aiding clinicians in making more informed decisions.
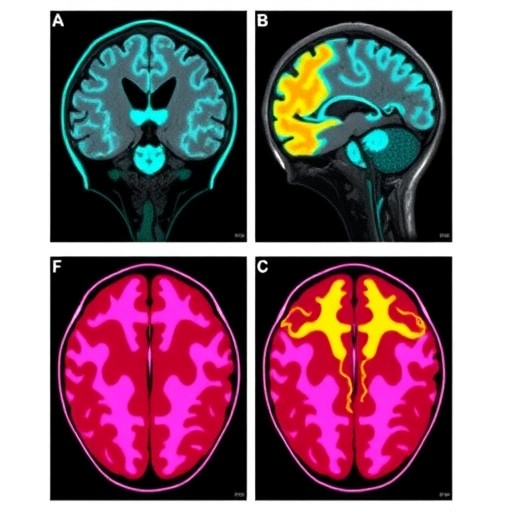
Neuroradiological imaging plays a pivotal role in diagnosing ECL, as it allows healthcare providers to visualize the extent of lipomatous tissue involvement in the central nervous system. Magnetic resonance imaging (MRI) and computed tomography (CT) scans are the primary tools utilized, offering enhanced delineation of the lipomas and associated brain anomalies. Through these imaging modalities, clinicians can assess the structural integrity of the brain and understand the potential neurological impacts, which differ from patient to patient.
.adsslot_8Riy0Sk9e2{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_8Riy0Sk9e2{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_8Riy0Sk9e2{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
The cutaneous manifestations of ECL can vary from simple, superficial lipomas to more complex lesions involving deeper tissues. These skin findings often provide the first clue to the diagnosis, and their careful assessment is essential. Dermatological examination combined with radiological assessment allows for a comprehensive evaluation, ensuring both the physical and psychological impacts of ECL are addressed through collaborative care.
Histopathological evaluation is another critical component in understanding ECL. Biopsies of cutaneous lesions can reveal the presence of mature adipose tissue, which is indicative of the disorder. This histopathological confirmation not only solidifies the diagnosis but also serves to distinguish it from other neurocutaneous syndromes that may exhibit similar clinical features, thereby refining the diagnostic process.
Genetic research has also emerged as a significant facet of understanding ECL. Although most cases are sporadic, identifying any potential underlying genetic mutations could provide insight into the pathogenesis of the disorder. Advances in genomic studies may eventually lead to the development of targeted therapies that could mitigate some of the symptoms associated with this challenging condition.
Neuropsychological evaluations are essential, particularly for children impacted by ECL. Cognitive assessments can help identify areas where developmental interventions are necessary, ensuring a holistic approach to treatment that encompasses both physical and mental health. These evaluations can highlight the need for supportive therapies, as children with ECL may experience challenges in learning and social interactions.
Therapeutic strategies for ECL should be multidisciplinary, incorporating contributions from dermatologists, neurologists, and psychologists. Surgery may be considered for significant lipomas that pose compressive threats to neurological function. However, given the rare nature of the condition, surgical intervention should be carefully considered against potential risks and benefits.
Long-term follow-up is crucial in managing patients with ECL, as new symptoms can emerge over time, necessitating ongoing assessments. Regular imaging and clinical evaluations can help identify changes in the condition, facilitating timely interventions. Notably, raising awareness among healthcare providers is critical for early detection, which can profoundly affect outcomes.
In summary, Encephalocraniocutaneous lipomatosis remains a complex disorder requiring a nuanced understanding of its neurocutaneous manifestations. Enhanced imaging technologies and interdisciplinary approaches contribute to improved management and outcomes for those affected. As research continues, it holds the promise of uncovering further insights into this rare condition, potentially leading to innovations in diagnosis, treatment, and overall patient care.
As health professionals delve deeper into the intricacies of ECL, the importance of patient-centered care cannot be overstated. Supportive networks involving family members, educators, and medical communities play a vital role. These networks not only provide essential emotional support but also foster understanding and acceptance, promoting the overall well-being of those affected by ECL, who may feel isolated due to their unique medical challenges.
In conclusion, the growing body of research surrounding Encephalocraniocutaneous lipomatosis underscores the need for increased awareness and understanding of this rare disorder. As more information emerges, the interdisciplinary collaboration among healthcare providers will be paramount. This collaboration will ensure that advancements in treatment and management strategies are effectively implemented, ultimately enhancing the quality of life for patients burdened by this complex condition.
In light of these advancements, the future appears hopeful for individuals suffering from ECL. Researchers and clinicians are committed to unraveling the complexities of this disorder, and ongoing studies are expected to yield even more profound insights that will pave the path for improved outcomes and potentially even preventative approaches.
Subject of Research: Encephalocraniocutaneous lipomatosis
Article Title: Encephalocraniocutaneous lipomatosis—a neuroradiological perspective.
Article References: Patel, D., Gripp, K., Mcdunnah, P. et al. Encephalocraniocutaneous lipomatosis—a neuroradiological perspective. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06346-8
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06346-8
Keywords: Encephalocraniocutaneous lipomatosis, neurocutaneous disorders, neuroradiology, magnetic resonance imaging, genetic research, interdisciplinary approach, patient-centered care.
Tags: brain malformations in neurocutaneous disorderscortical dysplasia and seizuresCT scans for brain abnormalitiesdiagnosing rare neurocutaneous conditionsearly life symptoms of ECLEncephalocraniocutaneous lipomatosislipomas affecting brain structuresMRI in ECL diagnosisneuroanatomical implications of ECLneurocutaneous disordersneuroradiological imaging techniquestreatment planning for ECL