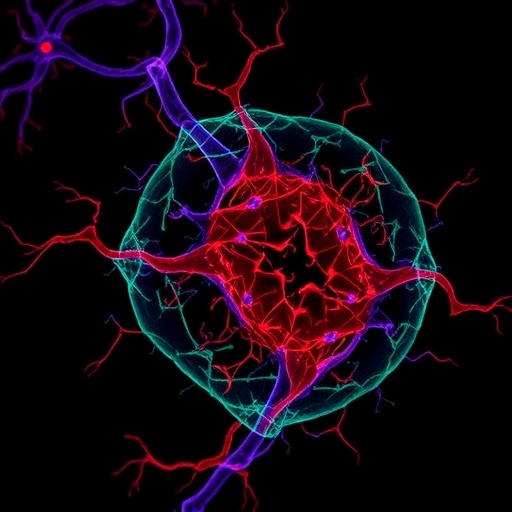
In recent years, the intricate relationship between the nervous system and immune regulation has sparked intense scientific interest, revealing layers of complexity previously underappreciated. While it is now well established that the peripheral nervous system (PNS) influences immune responses in various contexts, its direct impact on tumor immunity remains elusive. Groundbreaking research published in Nature by Baruch et al. (2025) sheds unprecedented light on this frontier, demonstrating how cancer-induced nerve injury (CINI) orchestrates resistance to anti-PD-1 immunotherapy—a cornerstone treatment modality in oncology.
The study presents a comprehensive analysis spanning patient-derived multiomic data, refined cell culture experiments, and sophisticated genetically engineered mouse models. This multifaceted approach uncovers a novel pathophysiological axis: invading cancer cells degrade the protective myelin sheath around peripheral nerves, eliciting nerve injury. This myelin damage disrupts normal nerve electrical conduction, confirmed through advanced structural and functional assays. This nerve injury acts as more than a collateral consequence; it sparks a cascade of neuronal stress signaling that profoundly remodels anti-tumor immunity.
Central to this process is the induction of ATF3, a transcription factor quintessential to the neuron injury response. ATF3 activation triggers upregulation of type I interferon (IFN-I) and interleukin-6 (IL-6) signaling within the neurons themselves. This neuron-intrinsic inflammatory signature does not remain isolated; it promotes recruitment and chronic infiltration of immunosuppressive, pro-healing immune cells into the perineural niche. The consequence is a local immune milieu that increasingly favors nerve repair and tumor tolerance at the expense of effective antitumor immunity.
.adsslot_bVMHzAxjdW{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_bVMHzAxjdW{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_bVMHzAxjdW{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The progression of malignant tumors intensifies this cycle by expanding their invasion into adjacent nerves, thereby amplifying the extent of CINI and sustaining the chronic inflammatory state. This vicious loop culminates in a tumor microenvironment (TME) that robustly suppresses immune responses critical for the success of immune checkpoint blockade therapies such as anti-PD-1. The study compellingly illustrates that this neuronal injury-driven inflammation undermines the efficacy of immunotherapies, offering a plausible explanation for treatment resistance seen in multiple cancer types exhibiting perineural invasion.
Experimental intervention targeting discrete nodes along the CINI pathway yielded promising therapeutic insights. Conditional knockout of Atf3 in neurons curtailed injury signaling, while genetic ablation of the IFN-I receptor Ifnar1 disrupted downstream inflammatory cascades. Additionally, antibody-mediated blockade of IL-6 pathways effectively reprogrammed the immunosuppressive perineural environment. These manipulations restored sensitivity to anti-PD-1 treatment in murine models, demonstrating that CINI-induced immunosuppression is amenable to pharmacological intervention.
Importantly, the authors distinguish the biological consequences of CINI from generalized cancer-induced cytotoxicity. The reduction in neuronal viability and aberrant signaling appears to correlate tightly with the presence of perineural invasion, underscoring the significance of specific cancer–nerve interactions rather than diffuse tumor burden. This nuanced understanding emphasizes that cancer’s invasive behavior—not merely its systemic effects—dictates the extent of nerve injury and immune modulation.
The in vitro co-culture models that simulate active perineural invasion further reinforce these findings. By fostering direct contact between cancer cells and neurons, the models revealed real-time dynamic interactions that drive neuronal stress responses and inflammatory signaling. This represents a significant advancement in dissecting the cellular cross-talk that underpins the CINI phenomenon and its immunological consequences.
Collectively, this research portrays a previously underappreciated mechanism wherein cancer remodels its microenvironment through hijacking nerve injury responses to evade immune eradication. It suggests that neurons are not passive bystanders but active modulators of tumor-immune interactions, capable of shaping the local immune contexture in favor of tumor survival. Such discoveries open novel avenues for biomarker identification and combinatorial therapeutic strategies aimed at overcoming anti-PD-1 resistance.
The implications of these findings extend beyond a single tumor type, as multiple cancers exhibiting perineural invasion may utilize this nerve injury-inflammation axis to subvert immune clearance. Targeting nerve injury pathways or their inflammatory sequelae could therefore represent a unifying therapeutic approach to enhance immunotherapy outcomes across diverse malignancies.
As cancer immunotherapy continues to revolutionize treatment paradigms, overcoming resistance mechanisms represents a critical challenge. The identification of CINI as a driver of immunosuppression provides a concrete target, heralding the development of adjunct therapies that may sensitize tumors to immune checkpoint blockade. Future investigations will be required to translate these insights into clinical applications and to characterize the long-term effects of modulating nerve-immune interactions within tumors.
In essence, Baruch and colleagues have spotlighted an elegant and complex dialogue between cancer cells and the nervous system, revealing how neuronal injury actively undermines cancer immunotherapy. Their breakthrough not only expands the conceptual framework of tumor immunology but also underscores the importance of studying the neuroimmune interface in cancer biology. This paradigm shift promises to stimulate broad scientific inquiry and accelerate progress toward more effective, durable cancer therapies.
Subject of Research: The effect of cancer-induced peripheral nerve injury on immune response and resistance to anti-PD-1 immunotherapy
Article Title: Cancer-induced nerve injury promotes resistance to anti-PD-1 therapy.
Article References:
Baruch, E.N., Gleber-Netto, F.O., Nagarajan, P. et al. Cancer-induced nerve injury promotes resistance to anti-PD-1 therapy. Nature (2025). https://doi.org/10.1038/s41586-025-09370-8
Image Credits: AI Generated
Tags: anti-PD-1 immunotherapy mechanismsATF3 transcription factor rolecancer-induced nerve injury researchgenetically engineered mouse models in oncologyinterleukin-6 signaling in tumorsmultiomic data in cancer researchmyelin sheath degradation in cancernerve injury and cancer resistanceneuron-intrinsic inflammatory responsesneuronal stress signaling in cancer treatmentperipheral nervous system and immunitytumor immunity and nerve interactions