New research from Memorial Sloan Kettering Cancer Center (MSK) identifies a promising immunotherapy target for acute myeloid leukemia; decodes genetic differences in tumors from patients with African ancestry; and finds a virtual mind-body fitness program reduced hospitalizations for those in active cancer treatment. A clinical trial led by MSK also resulted in the approval of a new combination therapy for non-small cell lung cancer.
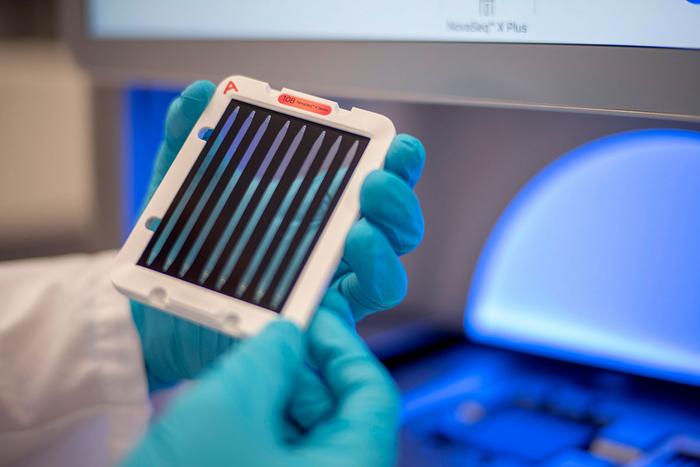
Credit: Memorial Sloan Kettering Cancer Center
New research from Memorial Sloan Kettering Cancer Center (MSK) identifies a promising immunotherapy target for acute myeloid leukemia; decodes genetic differences in tumors from patients with African ancestry; and finds a virtual mind-body fitness program reduced hospitalizations for those in active cancer treatment. A clinical trial led by MSK also resulted in the approval of a new combination therapy for non-small cell lung cancer.
MSK researchers identify promising immunotherapy target for AML
While immunotherapies have revolutionized the treatment of many cancers, they’ve largely been ineffective against acute myeloid leukemia (AML). That’s because the similarities between the cell surface proteins of healthy blood-forming cells and malignant cells make it difficult to selectively target just the cancer cells. Researchers at MSK, however, have taken an important step toward developing effective antibody-based immunotherapies for AML by identifying a unique, targetable antigen on the surface of AML cells. The work lead to new therapeutic antibodies, antibody-drug conjugates and chimeric antigen receptor (CAR) T cells.
Led by former hematology/oncology fellow Katherine Knorr, MD, PhD, and senior author Omar Abdel-Wahab, MD, Chair of the Molecular Pharmacology Program at the Sloan Kettering Institute, the research team reported promising results in targeting aberrant cell surface localization of the RNA helicase U5 snRNP200 in mouse models of AML, which were further improved by adding the chemotherapy drug azacitidine. “We are actively developing this approach as a therapeutic, and hope to launch a clinical trial within the next year or two,” Dr. Abdel-Wahab says. Read more in Nature Cancer.
Decoding genetic differences in tumors from patients with African ancestry
Tumor sequencing has become an important tool for diagnosing and treating cancer, but these tools may not benefit all patients equally. Less is known about the cancer genomes from people with African ancestry, especially compared with the cancer genomes from people of European ancestry. This may make it harder to pair certain patients with the best targeted therapies. Investigators at MSK are looking at ways to address and overcome these disparities. In a new study, they collaborated with researchers from several institutions in the US and Africa, using two large databases, including MSK-IMPACT®, to investigate the relationship between genomic alterations and African ancestry.
The team, led by computational geneticist Jian Carrot-Zhang, PhD, focused on six common cancers — lung, colorectal, breast, prostate, pancreatic, and ovarian. The genetic differences included: People with African ancestry diagnosed with lung, breast, and prostate cancers were more likely to have amplification of the gene MYC. Those with colorectal and pancreatic cancers were less likely to have BRAF alterations. In samples of lung cancer, researchers found several differences in clinically actionable mutations, such as ROS1 fusion enriched with African ancestry. They also showed how a history of smoking impacted the risk of TP53 mutations in people of African ancestry, providing evidence for tumorigenesis associated with ancestry-smoking interaction. The study suggests stronger efforts are needed to increase the representation of people with African ancestry in drug development and biomarker discovery, something the team plans to address. Read more in Cancer Cell.
Virtual mind-body fitness program reduced hospitalizations among patients undergoing active cancer treatments
A new interventional study found that participating in virtual mind-body fitness classes reduced hospitalizations, hospital stays, and urgent care visits for cancer patients in active treatment. The study was led by Jun Mao, MD, MSCE, chief of MSK’s Integrative Medicine Service and presented at the American Society of Clinical Oncology (ASCO) Quality Care Symposium in late October 2023.
The study involved 200 patients diagnosed with various cancers, including breast (36.5%), thoracic (24.5%), gynecologic (21.5%), head/neck (12.5%), or melanoma (5%), who had reported moderate or greater fatigue during active treatment. They were randomized into two groups. One group participated in the Integrative Medicine at Home (IM@Home) weekly virtual mind-body fitness classes featuring Integrative Medicine therapies such as fitness, meditation, yoga, tai chi, and music therapy. The second group received standard of care plus access to pre-recorded on-line meditation resources.
Those in the virtual mind-body fitness group were less likely to be hospitalized (5% vs. 14%) and spent fewer days in the hospital (5 days vs. 9 days) once they were admitted. Additionally, while the percentage of patients who needed to visit urgent care was similar was similar between groups, the number of urgent care visits per patient was almost half in the IM@Home group. Read the conference abstract.
New drug combination approved for non-small cell lung cancer
On October 11, 2023, the US Food and Drug Administration approved a combination of the targeted drugs encorafenib (Braftovi®) and binimetinib (Mektovi®) in patients with metastatic non-small cell lung cancer containing a mutation called BRAF V600E. The approval was based on a multicenter phase 2 clinical trial called PHAROS, which was led by MSK thoracic oncologists Gregory Riely, MD, PhD and Michael Offin, MD.
Encorafenib inhibits a cancer-causing protein called BRAF. Binimetinib inhibits a cancer-causing protein called MEK. The combination of the drugs, which are both taken as pills, was already approved for some people with melanoma. In the PHAROS trial, 44 of 59 patients with metastatic lung cancer responded to the drug combination, meaning that their tumors either shrank or stopped growing. For more than half of those who responded, the drugs were effective for at least a year. The rate of side effects for this drug combination was lower than what has been seen in other drug combinations targeting BRAF and MEK, making it a good option for patients whose lung cancer is caused by the BRAF V600E mutation. Findings from the trial were previously published in the Journal of Clinical Oncology.



