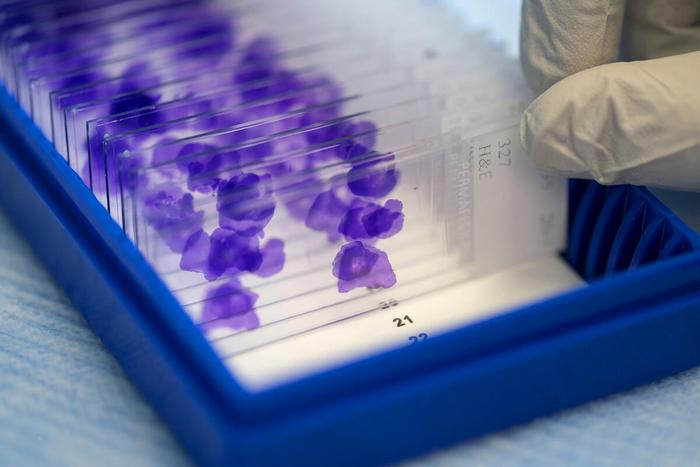
Most cancer types are identified by studying a sample under the microscope and through immunohistochemistry analysis, which looks for specific proteins in a tumor. For about 3-5% of patients, however — some 60,000 to 100,000 people per year — their cancer’s tissue of origin is unclear and can’t be used to guide treatment. An incorrect diagnosis, too, can lead to poor outcomes.
Credit: Memorial Sloan Kettering Cancer Center
MSK-developed deep-learning model designed to aid challenging cancer diagnoses
Most cancer types are identified by studying a sample under the microscope and through immunohistochemistry analysis, which looks for specific proteins in a tumor. For about 3-5% of patients, however — some 60,000 to 100,000 people per year — their cancer’s tissue of origin is unclear and can’t be used to guide treatment. An incorrect diagnosis, too, can lead to poor outcomes.
Now an MSK research team — overseen by molecular geneticist Michael Berger, PhD, of MSK’s Marie-Josée and Henry R. Kravis Center for Molecular Oncology, and computational biologist Quaid Morris, PhD, of the Sloan Kettering Institute — have developed a new, deep learning-based tumor-type prediction tool designed to aid identification. It applies artificial intelligence to cancer gene panel sequencing information to make predictions across 38 cancer types and supports the integration of additional patient-specific information to improve clinical decision making for challenging diagnoses. The team — led by study first author Madison Darmofal, a graduate student co-supervised by Dr. Berger and Dr. Morris — drew on a dataset of nearly 40,000 solid tumors sequenced using the MSK-IMPACT® gene panel to develop the Genome-Derived-Diagnosis Ensemble (or GDD-ENS). GDD-ENS, they report, made a high-confidence prediction in 72% of cases; among those, the accuracy rate was 93%. “Unlike previous studies indicating that tumor-type classifiers built on driver mutations alone have poor performance, we show that with sufficient training data set size, targeted gene panels can support highly accurate tumor-type classification,” the authors write. Read more in Cancer Discovery.
Researchers identify key regulators of infection-clearing immune cells
A collaboration between researchers at MSK and the University of California, San Francisco has identified key regulators of the ability of myeloid cells (like neutrophils and macrophages) to remove pathogens and cellular waste from the body — opening new possibilities for enhancing the body’s innate immunity in therapeutic contexts. The team found a specific G protein subunit called Gβ4 was important for controlling the behavior of a subset of myeloid cells called phagocytes. When Gβ4 was absent, the immune cells were more effective at engulfing and destroying cancer cells, fungi, bacteria, and other problematic cells. For example, they found mice whose neutrophils lacked Gβ4 were able to better clear a fungal infection. The enhanced phagocytic activity of Gβ4-deficient immune cells was caused by the expansion of their outer plasma membrane and involved a key lipid known as a sphingolipid. Targeting this mechanism could “be particularly useful for treating systemic microbial infections and for enhancing the antitumor potential of chimeric antigen receptor (CAR)–macrophages,” note the study authors, who include co-senior author Morgan Huse, PhD, an immunologist at the Sloan Kettering Institute and first author Benjamin Winer, PhD, a research scholar in the Huse Lab. “Exploring these possibilities in translationally relevant experimental systems will be an interesting topic for future research.” Read more in Science Immunology.
Research sheds new light on the mechanical forces exerted by immune cells
Conversations about the killing power of immune cells usually revolve around the chemical arsenal they wield against cancer cells and pathogens. But researchers at MSK’s Sloan Kettering Institute continue to shed light on the underappreciated role of mechanical forces exerted by immune cells. Using a technique called super-resolution traction force microscopy, a team co-led by graduate students Miguel Francisco de Jesus (who was recently awarded his doctorate) and Alexander Settle from the lab of immunologist Morgan Huse, PhD, found cytotoxic T cells form a compressive crater on target cells with complex, uneven surfaces. This pattern of forces was markedly different from those exerted by macrophages and by T cells performing other immune functions. They also found the strength and shape of the forces exerted by cytotoxic T cells was directly linked to their ability to kill target cells. These findings could help develop new strategies for modulating specific immune responses. Read more in Science Immunology.



