Recent advancements in the field of genetics have illuminated the intricate nature of mitochondrial disorders, specifically focusing on MPV17-related mitochondrial DNA depletion syndrome (MDDS). This condition is characterized by a reduction in mitochondrial DNA (mtDNA) and is linked to mutations in the MPV17 gene, which plays a crucial role in mitochondrial function. Mitochondria are often referred to as the powerhouses of the cell, providing the energy necessary for various biological processes. When they do not function properly, it can lead to a spectrum of clinical manifestations, particularly affecting organs with high energy demands such as the liver and brain.
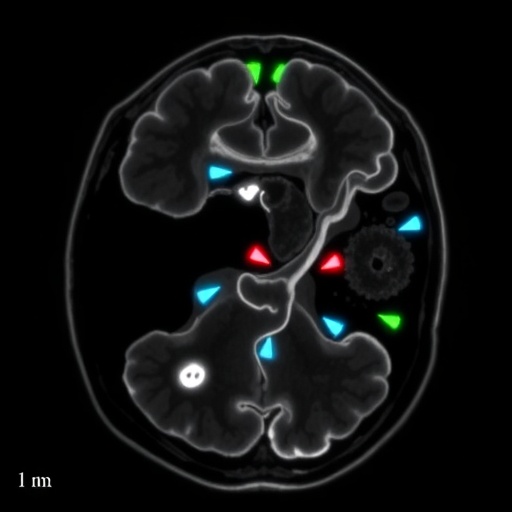
In a groundbreaking retrospective observational study, notable researchers O’Hagan, Meldau, and Rose et al. have shed light on the magnetic resonance imaging (MRI) features specific to this devastating condition. Their work, published in Pediatr Radiol, offers valuable insights that could not only enhance the diagnostic process but may also pave the way towards understanding the pathophysiological repercussions of MPV17 mutations on the brain’s architecture and function.
The crux of this research lies in the compelling correlation between genetic mutations and observable alterations in brain structure as revealed through MRI scans. Interestingly, the study cataloged a variety of MRI features that are predominantly associated with MPV17-related MDDS. Some of the notable findings detail changes in cerebral white and gray matter, which can often be overlooked in a clinical environment. By cataloguing such abnormalities, the authors aim to provide clinicians with a robust framework for recognizing MDDS during diagnostic assessment efficiently.
.adsslot_XoUeynbShu{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_XoUeynbShu{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_XoUeynbShu{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
One fascinating aspect of the research is the variety of ages at which these MRI anomalies can manifest. The featured cohort included children and adolescents, showcasing that the impact of the MPV17 mutation could introduce MRI abnormalities even in the early years of life. This emphasizes the necessity for early screening and intervention, as identifying these changes can lead to timely therapeutic strategies that may potentially mitigate further neurological decline.
Furthermore, the researchers outlined potential pathways that could be investigated to further understand the etiology of MDDS. Given that mitochondrial dysfunction is involved, a deeper exploration of the metabolic pathways affected by these MPV17 mutations may illuminate new therapeutic targets. Genetic screening could become an essential component of routine assessments in at-risk populations, thus reinforcing a proactive approach to managing mitochondrial diseases.
There is also a compelling call to action within this research, urging medical professionals to remain vigilant for signs of MDDS, particularly in patients who present with nonspecific neurological symptoms. The varied manifestations of this condition underscore the complexity of mitochondrial diseases and the necessity for comprehensive care encompassing not just physical assessments but also a thorough understanding of the patient’s genetic background.
The role of interdisciplinary collaboration is another pivotal theme presented in this study. The authors suggest that engaging with geneticists, neurologists, and radiologists as a collaborative team could ignite breakthroughs in how MDDS and similar mitochondrial disorders are understood and treated. By bridging the gap between genetics and clinical application, healthcare providers can ensure that patients receive holistic care focused on both physical and psychological health.
As researchers continue to unravel the complexities associated with mitochondrial DNA depletion syndromes, the results of this study serve as a beacon of hope. The detailed exploration of MRI features highlights a crucial intersection between technology and genetics, showcasing how advanced imaging can deliver monumental insights into conditions previously shrouded in ambiguity. This reinforces the concept that the integration of technological advancements into clinical practice can significantly streamline the diagnostic processes.
The lasting impact of this study cannot be understated. The findings not only cater to the current clinical landscape but also set a precedent for future research in genetic mitochondrial disorders. There is a palpable excitement within the scientific community as researchers look to expand on these findings, facilitating a deeper understanding that might one day lead to effective treatments or even therapeutic reversals for those living with such debilitating conditions.
The implications of MPV17-related MDDS extend beyond individual patients, touching families, support networks, and entire healthcare infrastructure. The emotional burden of such diagnoses can weigh heavily on families as they navigate the complexities of care while grappling with uncertain prognoses. Therefore, the enhanced diagnostic accuracy afforded by this study could not only foster improved individual health outcomes but also bring peace of mind to families seeking clarity in a tumultuous situation.
In summation, the meticulous work spearheaded by O’Hagan, Meldau, and Rose et al. represents a significant stride forward in the understanding of MPV17-related mitochondrial DNA depletion syndrome. Their research provides a foundation upon which future studies can build, nurturing a multidisciplinary approach toward tackling the multifaceted challenges posed by mitochondrial disorders. With each new finding, the path toward innovative therapies and improved patient care becomes increasingly illuminated, heralding a new era in mitochondrial medicine.
As this research garners attention, it is essential for the scientific community to proactively disseminate these findings, inspiring further inquiry and innovation in the field. The quest for answers surrounding mitochondrial disorders is far from complete; however, with the contributions of pioneering researchers and clinicians alike, a brighter and more informed future is assured for those affected by these challenging conditions.
Subject of Research: Magnetic resonance imaging features of MPV17-related mitochondrial DNA depletion syndrome.
Article Title: Retrospective observational study of the magnetic resonance imaging features of MPV17-related mitochondrial DNA depletion syndrome.
Article References: O’Hagan, S., Meldau, S., Rose, P. et al. Retrospective observational study of the magnetic resonance imaging features of MPV17-related mitochondrial DNA depletion syndrome. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06341-z
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06341-z
Keywords: MPV17, mitochondrial DNA depletion syndrome, MRI, genetic disorders, pediatric radiology.
Tags: advancements in genetic researchbrain architecture and mitochondrial disordersclinical manifestations of mitochondrial diseasediagnostic imaging in mitochondrial diseasesgenetic mutations and brain structuremitochondrial DNA depletion syndromemitochondrial function and energy productionMPV17-related mitochondrial diseaseMRI features of mitochondrial disorderspathophysiological effects of MPV17 mutationspediatric radiology insightsretrospective observational study in medicine