In a groundbreaking study set to reshape the understanding of inflammatory bowel disease (IBD) in pediatric patients, researchers have identified significant hepatobiliary and pancreatic findings through magnetic resonance enterography (MRE). This imaging technology has emerged as a critical tool in the diagnosis and management of inflammatory bowel conditions, enhancing the accuracy and depth of the assessments available to clinicians. The research, led by an experienced team, including L. Scheller, J. Dillman, and K. Epstein, offers novel insights into the complex interplay between gastrointestinal and hepatobiliary health in children afflicted with IBD.
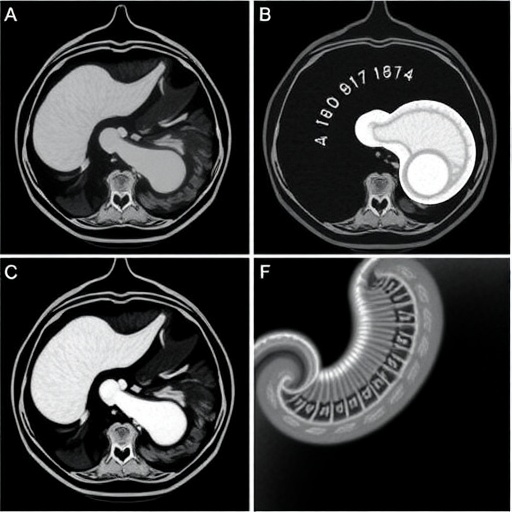
The significance of this study cannot be overstated, as it elucidates the often-overlooked aspects of hepatobiliary and pancreatic pathologies concomitant with inflammatory bowel disease. MRE has gained traction as a non-invasive modality, providing vivid images that can pinpoint abnormalities, differentiate between various forms of IBD, and showcase organ involvement. In the context of pediatric patients, these findings are particularly crucial, considering the long-term implications of uncontrolled inflammation that can lead to substantial morbidity.
The preliminary outcomes of this research reveal an intriguing association between the severity of IBD and the presence of changes in the hepatobiliary system. Through the comprehensive examination of MRE images, it appears that children with newly diagnosed IBD frequently exhibit alterations in their liver and pancreatic structures, which can serve as a precursor to potential complications if not managed appropriately. This raises essential questions about routine imaging practices and the necessity for an interdisciplinary approach involving pediatric gastroenterologists and radiologists.
Meticulously examining the datasets collected from various pediatric patients, the research team found that there is varied presentation among individuals with IBD regarding hepatobiliary findings. These discrepancies underscore the heterogeneous nature of the disease, which can manifest differently across various demographics and genetic backgrounds. The capability of MRE to detect these nuances plays a pivotal role in tailoring individualized treatment plans, highlighting the importance of personalized medicine in the realm of IBD management.
Inflammatory bowel disease is notoriously difficult to diagnose, especially in children, due to overlapping symptoms with other gastrointestinal disorders. The introduction of advanced imaging techniques like magnetic resonance enterography into clinical practice brings a glimmer of hope, as it potentially shortens the diagnostic timeline. This transformation is vital in ensuring timely intervention, preventing unnecessary complications, and improving overall quality of life for pediatric patients suffering from IBD.
In addition to the immediate benefits of accurate diagnosis, these findings could suggest a paradigm shift in our understanding of disease progression and management strategies. The implications of detecting hepatobiliary and pancreatic involvement early on may prompt clinicians to adopt more aggressive treatment regimens aimed at controlling inflammation and mitigating the risk of further organ damage. Such approaches may ultimately foster better health outcomes and longitudinal success in managing IBD from a young age.
Moreover, the research opens avenues for further exploration into the connection between diet, lifestyle factors, and the emergence of hepatobiliary anomalies in children with IBD. Understanding the underlying mechanisms of such associations may lead to the development of preventive strategies that extend beyond pharmacological intervention. As awareness increases and clinical practice evolves, the groundwork laid by this study provides a launching pad for future investigations aimed at unraveling the complexities of gut-associated liver diseases in pediatric populations.
Another critical element of the study revolves around patient education and empowerment. As healthcare systems emphasize the role of shared decision-making, the findings from MRE should engage families to participate in discussions about their child’s health actively. Providing parents with insights into the potential complications linked with untreated liver and pancreatic changes promotes a collaborative framework focused on the health and well-being of the child.
The article, set to be published in the renowned journal Pediatrics Radiology, represents a significant scientific contribution to the field. Its findings are likely to resonate widely, fostering discussions at conferences and fueling debates in medical circles. The call for further research and consensus on the management of hepatobiliary and pancreatic findings in pediatric IBD populations will become increasingly important as practitioners strive for excellence in care delivery.
In summary, the combination of advanced imaging techniques like magnetic resonance enterography and a detailed examination of hepatobiliary and pancreatic findings in children newly diagnosed with inflammatory bowel disease marks a pivotal moment in pediatric gastroenterology. The implications of this research are bound to affect clinical practices, inform treatment paradigms, and above all, elevate the standard of care for vulnerable populations facing chronic and relapsing conditions. As more pediatric patients are diagnosed with IBD, the importance of integrating comprehensive imaging approaches is clearer than ever.
This research underscores the critical need for a holistic approach, combining cutting-edge diagnostic tools with innovative treatment strategies and coordinated care. The excitement surrounding these findings is palpable, and the potential for transforming patient outcomes is firmly within reach.
As we await long-term follow-ups and additional studies to validate these initial findings, it is the hope of the research community that this exploration of hepatobiliary and pancreatic involvement in pediatric inflammatory bowel disease will ignite a renaissance in understanding this challenging disease, ultimately aiding in the development of robust treatment protocols for future patients.
Subject of Research: Hepatobiliary and pancreatic findings in children with newly diagnosed inflammatory bowel disease.
Article Title: Hepatobiliary and pancreatic findings on magnetic resonance enterography examinations in children with newly diagnosed inflammatory bowel disease.
Article References:
Scheller, L., Dillman, J., Epstein, K. et al. Hepatobiliary and pancreatic findings on magnetic resonance enterography examinations in children with newly diagnosed inflammatory bowel disease.
Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06463-4
Image Credits: AI Generated
DOI: 19 November 2025
Keywords: Inflammatory bowel disease, pediatric gastroenterology, magnetic resonance enterography, hepatobiliary findings, pancreatic involvement, diagnosis, treatment strategies.
Tags: associations between IBD severity and liver changescomprehensive imaging for IBD assessmenthepatobiliary findings in childrenimplications of IBD on liver healthmanaging inflammatory bowel disease in pediatric patientsMR enterography in IBD diagnosisMRE technology in pediatric medicinenon-invasive imaging techniques for IBDnovel insights into pediatric gastrointestinal healthpancreatic abnormalities in pediatric IBDpediatric inflammatory bowel diseaseresearch on gastrointestinal diseases in children