In a groundbreaking advancement that promises to transform therapeutic strategies for muscle-invasive bladder cancer (MIBC), researchers at the Icahn School of Medicine at Mount Sinai have unveiled compelling evidence supporting the use of ultra-sensitive molecular assays to guide bladder-sparing treatment approaches. This study, recently published in the prestigious Proceedings of the National Academy of Sciences, elucidates how precision detection of tumor-derived DNA in blood and urine can critically inform which patients may safely avoid radical cystectomy, a procedure long regarded as the standard, yet life-altering, treatment for this aggressive malignancy.
Muscle-invasive bladder cancer, characterized by the invasion of tumors into the muscular wall of the bladder, has traditionally necessitated a treatment regimen starting with systemic chemotherapy followed by radical cystectomy — the complete surgical removal of the bladder. While effective in oncological control, cystectomy imposes profound impacts on patient quality of life, mandating urinary diversion and often precipitating physical and psychological morbidity. Paradoxically, extensive clinical experience has revealed that a significant subset of these patients exhibit no residual viable cancer at the time of surgery, implying that some may be overtreated under current protocols.
The research team, led by Dr. Matthew D. Galsky at Mount Sinai, aimed to refine treatment paradigms through nuanced molecular diagnostics capable of identifying minimal residual disease (MRD). By analyzing circulating tumor DNA (ctDNA) in plasma and urine tumor DNA (utDNA) in urine—a fragmentary genetic signature shed by malignant cells into bodily fluids—they sought to develop a non-invasive biomarker strategy that could reliably differentiate patients harboring occult disease from those achieving complete response to chemotherapy.
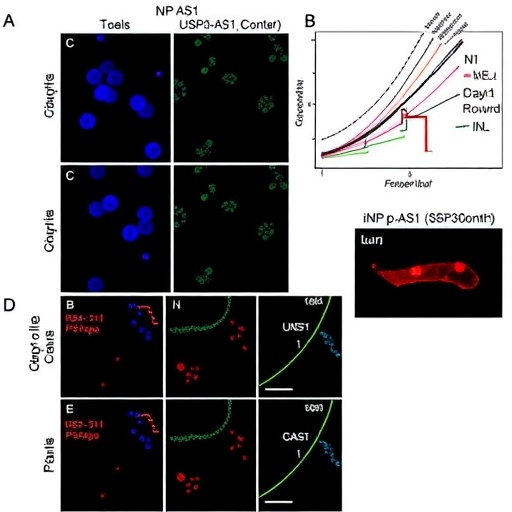
This observational study leveraged samples from a clinical trial cohort undergoing bladder-sparing interventions. Patients who demonstrated a complete clinical response, verified by comprehensive diagnostic modalities including bladder biopsy, were assessed for residual disease using the ctDNA and utDNA assays. Collaborating with Dr. Bert Vogelstein and his team at Johns Hopkins University, pioneers in ctDNA MRD research, the investigators employed cutting-edge molecular techniques to achieve ultra-sensitive detection thresholds, revealing critical prognostic insights.
Strikingly, the study reported that patients with undetectable ctDNA or utDNA post-treatment had a markedly favorable prognosis, with three-year bladder-intact survival rates nearing 69 percent. This compelling evidence supports the feasibility of forgoing immediate cystectomy in carefully selected individuals without compromising oncological safety, heralding a paradigm shift towards personalized, organ-preserving care in MIBC.
Moreover, plasma ctDNA detection before systemic therapy emerged as a potent predictive biomarker for metastatic progression. Patients presenting with baseline ctDNA positivity faced significantly heightened risk of developing distant disease, underscoring its utility for risk stratification and guiding therapeutic intensification. Conversely, those without detectable ctDNA at baseline exhibited remarkably low rates of metastatic recurrence, emphasizing the assay’s prognostic precision.
Complementing plasma ctDNA, analysis of urine tumor DNA revealed enhanced sensitivity in detecting residual disease localized within the bladder. Notably, patients who had no clinical or histological evidence of cancer yet demonstrated detectable utDNA experienced poorer bladder-intact survival, suggesting that urine-based liquid biopsy captures microscopic, clinically occult disease that conventional assessments may overlook.
Dr. Galsky emphasized the synergy of dual-compartment molecular monitoring: “Our findings illuminate how plasma and urine tumor DNA assays provide complementary, actionable information. By integrating these liquid biopsy modalities, we can more accurately identify patients who stand to benefit most from bladder preservation without risking compromised cancer control.”
The implications of these findings extend beyond immediate clinical application; they chart a course towards integrating molecular diagnostics into real-time decision-making for bladder cancer management. Radical cystectomy, while curative for many, remains an invasive surgery associated with substantial morbidity and lifestyle alterations. The ability to confidently spare patients from unnecessary surgery through precise biomarker guidance represents a monumental stride in oncologic care, advancing the imperative for de-escalation strategies anchored in robust molecular evidence.
Importantly, this study serves to validate and expand upon the pioneering foundational work of Dr. Vogelstein and collaborators, who first established ctDNA as a viable biomarker for MRD in solid tumors. The current Mount Sinai-led investigation enhances this paradigm by incorporating urine tumor DNA analysis and applying these technologies in a clinically relevant bladder-sparing trial context.
Future directions will necessitate validation of these assays in larger multi-institutional cohorts and prospective clinical trials aimed at embedding ctDNA and utDNA monitoring into standardized treatment algorithms. Such efforts will be crucial to confirm reproducibility, optimize assay sensitivity and specificity, and ascertain long-term oncologic outcomes attendant to biomarker-driven management.
The multidisciplinary collaboration underpinning this research—including experts in medical oncology, urology, pathology, genomics, and bioinformatics—from institutions such as the University of Michigan, City of Hope, Oregon Health & Science University, USC Keck School of Medicine, University of Pennsylvania, and the University of Wisconsin—reflects the complexity and innovation required to bring precision oncology to the forefront of bladder cancer care.
As molecular diagnostics and targeted therapies continue to evolve, the current research exemplifies a pivotal movement away from uniform, invasive treatment towards tailored interventions that prioritize both survival and quality of life. The precise detection of circulating tumor DNA markers heralds a new era whereby clinicians can more confidently distinguish between patients in genuine need of radical intervention and those who may be effectively cured with conservative, bladder-sparing strategies.
Dr. Galsky concluded, “This study is an essential advance towards truly individualized therapy for muscle-invasive bladder cancer. We envision a future in which molecular monitoring empowers clinicians to avoid overtreatment and preserve patient dignity without sacrificing clinical outcomes. As we validate these findings across diverse populations, the integration of liquid biopsies into standard practice holds immense promise for reshaping bladder cancer treatment globally.”
Subject of Research: Human tissue samples
Article Title: Monitoring of plasma and urine tumor-derived DNA to inform bladder-sparing approaches for patients with muscle-invasive bladder cancer
News Publication Date: February 18, 2026
Web References: http://dx.doi.org/10.1073/pnas.2533449123
References: Proceedings of the National Academy of Sciences (PNAS), DOI: 10.1073/pnas.2533449123
Keywords: Metastasis, circulating tumor DNA, urine tumor DNA, muscle-invasive bladder cancer, minimal residual disease, liquid biopsy, bladder preservation, radical cystectomy, personalized oncology
Tags: advancements in bladder cancer therapyavoiding radical cystectomy in MIBCbladder cancer and personalized treatment strategiesbladder-sparing therapy for bladder cancermolecular diagnostics for bladder cancermuscle-invasive bladder cancer treatmentnon-invasive bladder cancer monitoringpostoperative cancer monitoring techniquesprecision medicine in bladder cancerquality of life after bladder cancer treatmenttumor-derived DNA blood test for cancerultra-sensitive molecular assays in cancer detection