New largescale study in the American Journal of Preventive Medicine found overprescription of opioids by dentists common, particularly to patients at high risk for substance abuse, and that almost 1/3 of patients received more powerful drugs than needed
Credit: Michelle S. Woods
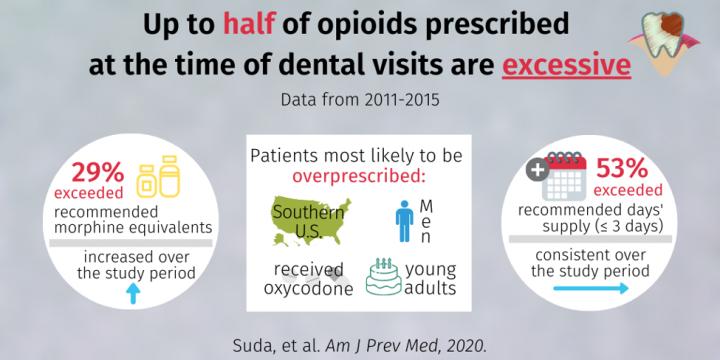
Ann Arbor, February 4, 2020 – Dentists are among top prescribers of opioids in the US, however, whether their opioid prescribing exceeds guidance had not been investigated. A new study in the American Journal of Preventive Medicine, published by Elsevier, indicates that more than half of opioid prescriptions issued by dentists exceed the three-day supply recommended by the US Centers for Disease Control and Prevention (CDC) for acute dental pain management. The findings also show that 29 percent of dental patients received more powerful opioids than needed for expected post-procedure pain.
“Unlike national trends, opioid overprescribing by dentists is increasing. Our results should initiate a call to action to professional organizations and public health and advocacy groups to improve the guidelines for prescribing opioids for oral pain. As high prescribers of opioids writing prescriptions for a tenth of the opioids dispensed in the US, dentists should be included as part of the multi-faceted solution needed for the opioid epidemic,” explained lead investigator Katie J. Suda, PharmD, MS, Professor, University of Pittsburgh School of Medicine, Division of General Internal Medicine, Pittsburgh, PA, USA.
The study used Truven Health MarketScan Research Databases to assess close to 550,000 dental visits by adult patients between 2011 and 2015, prior to the implementation of the 2016 CDC guidelines for pain management. These guidelines recommend first-line treatment using non-opioid analgesics for oral pain when possible. If stronger analgesics are needed after dental surgery, low-potency opioids (e.g., acetaminophen with codeine) are recommended instead of high-potency opioids (e.g., oxycodone). Moreover, three days or less of treatment is considered sufficient for typical oral pain. It is also a best practice for dentists to check their local prescription drug monitoring program (PDMP) before they write a prescription for any opioid to identify patients at risk of opioid abuse.
Investigators also found that the proportion of prescribed opioids that exceeded the recommended morphine equivalents increased in 2015. This was likely due to an increase in the quantity of hydrocodone tablets dispensed after the Food and Drug Administration’s (FDA) rescheduling of hydrocodone from a schedule III to a schedule II drug in 2014. While hydrocodone rescheduling was associated with a decrease in hydrocodone prescribing nationally, this study’s results suggest that this change resulted in an average increase of two tablets dispensed per hydrocodone prescription prescribed by dentists. Nationally, this increase translates to more than14 million additional hydrocodone tablets dispensed to patients after rescheduling hydrocodone to a schedule II drug.
“Similar to medical providers, dentists need to be provided resources to aid in their prescribing decisions for pain medications,” commented Dr. Suda. “This should include clinical guidelines specific to oral pain and education on how to talk to their patients about treating their oral pain.”
Co-investigator Susan A. Rowan, DDS, College of Dentistry, University of Illinois at Chicago, Chicago, IL, USA, emphasized that the demographic groups most impacted by overprescribing (patients aged 18 to 34 years, men, those living in the Southern US, and those receiving oxycodone) also carry a higher risk of addiction and overdose. She suggested that “additional studies are needed to evaluate the efficacy of the CDC 2016 prescribing guidelines subsequent to their introduction.”
“Future studies and targeted efforts to reduce overprescribing would also be well motivated among older patients and others taking multiple other high risk medications such as benzodiazepines,” added Gregory S. Calip, PharmD, MPH, PhD, College of, Pharmacy, University of Illinois at Chicago, Chicago, IL, USA.
Dr. Suda and co-investigators invite professional organizations and public health and advocacy groups to use the study’s data to inform future efforts. In the interim, they recommend that individual dentists implement their own practice-specific guidelines, favoring ibuprofen plus acetaminophen and low-potency opioids for post-extraction pain management.
Using statistical modeling, investigators predict that overprescribing would decrease by more than 20 percent if oxycodone prescriptions were substituted with lower potency opioids (such as hydrocodone).
###
Media Contact
Jillian B. Morgan, MPH
[email protected]
734-936-1590
Related Journal Article
http://dx.




