Credit: Jarrod Predina, Andrew Newton, Charuhas Deshpande, and Sunil Singhal of The Perelman School of Medicine at the University of Pennsylvania, and Philip Low of Purdue University
BELLINGHAM, Washington, USA, and CARDIFF, UK — In a proof-of-principle case report, researchers announce that targeted fluorescence successfully identified pulmonary metastases in a patient with osteosarcoma, making it easier for surgeons to locate the tumors for resection. This advance is reported in an article published today by SPIE, the international society for optics and photonics.
The case study "Utilization of targeted near-infrared molecular imaging to improve pulmonary metastasectomy of osteosarcomas," by Jarrod Predina, Andrew Newton, Charuhas Deshpande, and Sunil Singhal of The Perelman School of Medicine at the University of Pennsylvania, and Philip Low of Purdue University, is notable for its impact on osteosarcoma resection, according to the journal's editor-in-chief, Brian Pogue.
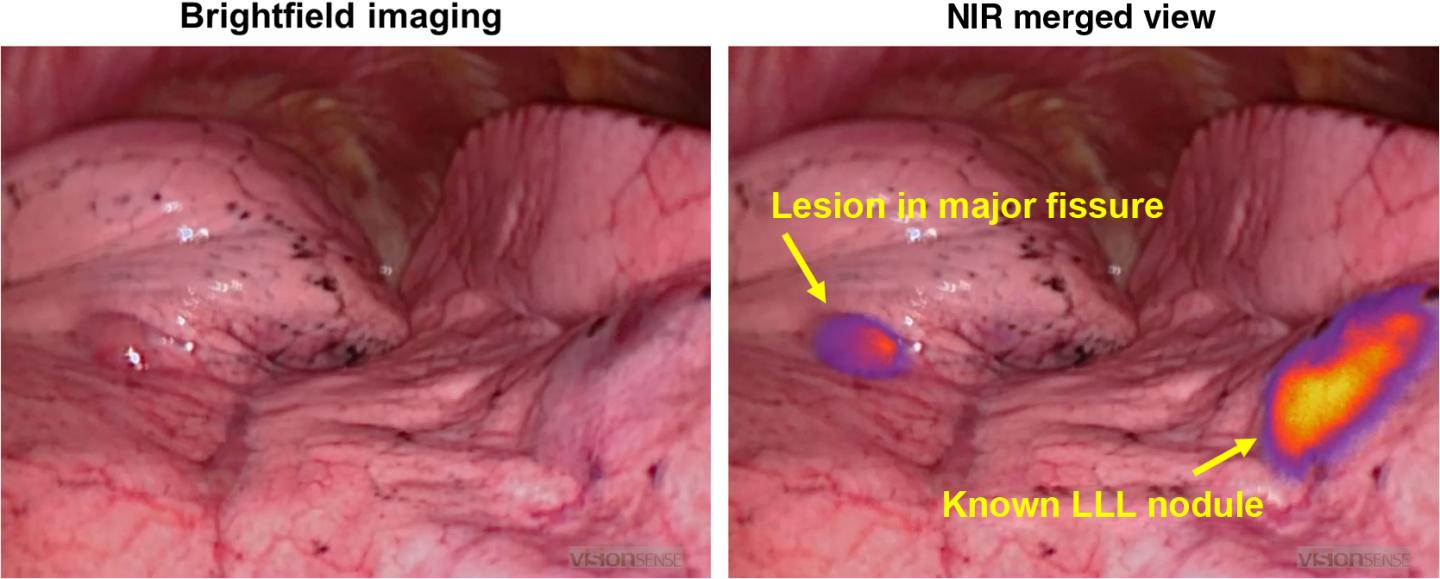
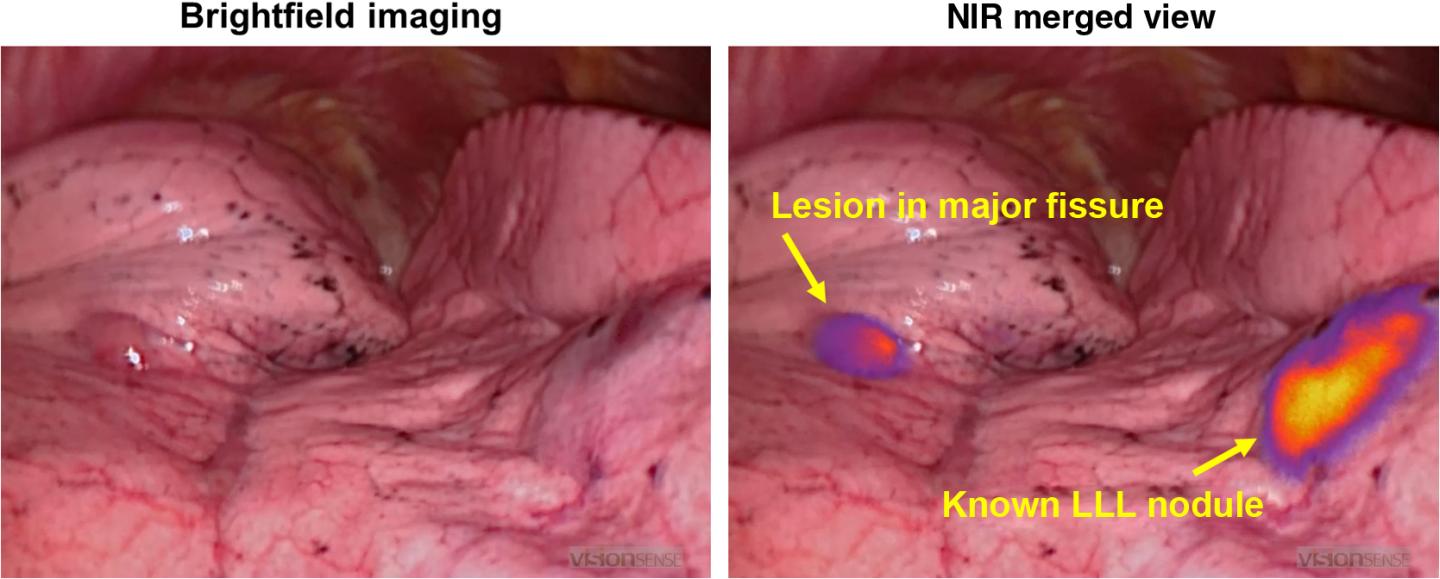
Osteosarcomas express a number of unique molecular markers, including the folate receptor alpha (FRα). This study utilized a near-infrared contrast agent known as OTL38, which binds to pulmonary metastases expressing FRα, and emits in the NIR range.
In this study, the fluorescence emitted from the contrast agent allowed surgeons to locate both a known lung nodule and a small occult metastases–less than a half a centimeter–that was not visible in preoperative imaging, suggesting that this approach may enable the detection of small or hard-to-locate nodules during minimally invasive resection.
The drug was safely delivered and no toxicity was observed, the authors reported. Both nodules were successfully resected using real-time fluorescence feedback.
The authors report that this technique may enhance the surgeon's ability to perform a variety of oncologic procedures including tumor localization, margin assessment, and intraoperative staging.
"The authors were able to examine the spatial heterogeneity of the folate-dye uptake and show that even though there is a complex uptake pattern, the shapes were representative of the underlying pathology distribution, and therefore provide a reasonable molecular tag for resection margins," said Brian Pogue.
Initial reports indicate that more than 90% of primary lung cancers accumulate OTL38 and generate tumor fluorescence during minimally invasive pulmonary resection, suggesting that this technique may have application beyond pulmonary osteosarcoma. Future research will explore if this approach could be applicable to other pulmonary malignancies that express the FRα.
###
Brian Pogue, Professor of Engineering at Thayer School of Engineering at Dartmouth, became the editor-in-chief of the Journal of Biomedical Optics on January 1, 2018. The journal is published in print and digitally by SPIE in the SPIE Digital Library, which contains more than 460,000 articles from SPIE journals, proceedings, and books, with approximately 18,000 new research papers added each year. The journal will become fully open access on January 1, 2019.
About SPIE
SPIE is the international society for optics and photonics, an educational not-for-profit organization founded in 1955 to advance light-based science, engineering, and technology. The Society serves nearly 264,000 constituents from approximately 166 countries, offering conferences and their published proceedings, continuing education, books, journals, and the SPIE Digital Library. In 2017, SPIE provided more than $4 million in support of education and outreach programs. http://www.spie.org
Media Contact
Kevin Probasco
[email protected]
360-685-5525
@SPIEtweets
http://spie.org/
Original Source
http://spie.org/x128342.xml http://dx.doi.org/10.1117/1.JBO.23.1.016005