Substantial differences in Medicaid compensation for standard-of-care breast cancer treatment indicate larger trend in cancer care
Credit: Elsevier
ARLINGTON, Va., April 11, 2019 — A new study finds wide state-by-state variations in Medicaid reimbursements to physicians who treat cancer patients with radiation therapies. These differences could compound existing disparities in access to health care in rural communities, which tend to have higher Medicaid coverage rates than metropolitan areas. The study is available for free access through April 24 in the International Journal of Radiation Oncology * Biology * Physics (Red Journal), the flagship scientific journal of the American Society for Radiation Oncology (ASTRO).
“Roughly 66 million low-income Americans are enrolled in Medicaid, and we know from previous studies that these patients face disproportionate difficulty and delays getting the care they need,” said Ankit Agarwal, MD, MBA, first author of the study and a radiation oncology resident physician at the University of North Carolina at Chapel Hill. “With cancer care, timely treatment matters, and states that under-compensate for radiation therapy likely undermine patients’ health outcomes.”
For the analysis, researchers examined 2017 Medicaid fee schedules from 48 states and the District of Columbia1. Key findings included:
- Fivefold difference in reimbursement rates: The average reimbursement for standard-of-care radiation therapy to treat breast cancer2 ranged from a low of $2,945 in New Hampshire, to a high of $15,218 in Delaware, with an overall average of $7,233 for an entire episode of care.
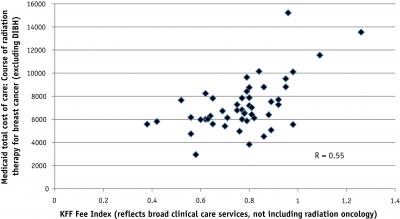
- Radiation oncology disproportionately affected: The variation in radiation therapy payments outpaces the differences seen with other Medicaid reimbursements. Analysis of the Kaiser Family Foundation Medicaid-to-Medicare fee index for general medical services found that reimbursement ratios ranged from a low of 0.38 in Rhode Island to a high of 1.26 in Alaska – a threefold difference. By comparison, the authors’ index of radiation oncology payments showed a fivefold difference.
“Clinics that provide radiation therapy also have expensive fixed costs to purchase and maintain the equipment used for treatments. Inadequate and disproportionate Medicaid reimbursement rates – which already fall below comparable Medicare rates – can negatively impact the viability of facilities, especially in rural and private practice settings. Any reduction in the number of facilities in these areas can limit or remove patient access to these life-saving medical services,” explained Dr. Agarwal.
“Greater stability and fairness in Medicaid compensation would help stabilize access for Medicaid patients and make it more financially feasible for the physicians who care for them, especially in rural communities and those with fewer physicians overall. If left unaddressed, however, the disparity could aggravate the growing maldistribution of radiation oncologists in rural and urban communities – and place low-income patients in rural communities at even greater threat.”
###
For a copy of the journal article or to arrange an interview with Dr. Agarwal, contact ASTRO’s media relations team at [email protected] or 703-286-1600.
1Findings are based on Medicaid fee schedules from the fourth quarter of 2017, obtained from the state Medicaid websites or departments. Two states were not included in the analysis: Tennessee does not follow a Medicaid fee-for-service model, and Illinois’ fee schedule was incomplete.
2The reference case was a patient who received hypofractionated radiation therapy for breast cancer, using the deep inspiration breast hold (DIBH) technique and a radiation boost to the tumor bed. This clinical scenario is one of the most common in radiation oncology; Dr. Agarwal also noted that reimbursement for this treatment scenario is generally reflective of how radiation oncology is reimbursed for other commonly-treated sites.
Article Details
- Title: Variations in Medicaid Payment Rates for Radiation Oncology
- Authors: Ankit Agarwal, MD, MBA; Jessica Peterson, MD, MPH; Lesley Hoyle, BS, RT, CMD; Lawrence B. Marks, MD, FASTRO
- International Journal of Radiation Oncology * Biology * Physics, Volume/Issue TBD
- https://www.redjournal.org/article/S0360-3016(19)30257-3/, DOI: doi.org/10.1016/j.ijrobp.2019.02.031
- The authors reported no conflicts of interest nor funding for this study.
ABOUT ASTRO
The American Society for Radiation Oncology (ASTRO) is the world’s largest radiation oncology society, with more than 10,000 members who are physicians, nurses, biologists, physicists, radiation therapists, dosimetrists and other health care professionals who specialize in treating patients with radiation therapies. The Society is dedicated to improving patient care through professional education and training, support for clinical practice and health policy standards, advancement of science and research, and advocacy. ASTRO publishes three medical journals, International Journal of Radiation Oncology * Biology * Physics, Practical Radiation Oncology and Advances in Radiation Oncology; developed and maintains an extensive patient website, RT Answers; and created the nonprofit foundation Radiation Oncology Institute. To learn more about ASTRO, visit our website, sign up to receive our news and follow us on our blog, Facebook, Twitter and LinkedIn.
Media Contact
Liz Gardner
[email protected]
Related Journal Article
http://dx.