Physicians currently use assessments like heart chamber size and systolic function to diagnose and monitor cardiomyopathy and other related heart conditions. A paper publishing in the journal Med on March 29 suggests that another measurement—cardiac sphericity, or roundness of the heart—may one day be a useful implement to add to the diagnostic toolkit.
Credit: Med/Vukadinovic et al.
Physicians currently use assessments like heart chamber size and systolic function to diagnose and monitor cardiomyopathy and other related heart conditions. A paper publishing in the journal Med on March 29 suggests that another measurement—cardiac sphericity, or roundness of the heart—may one day be a useful implement to add to the diagnostic toolkit.
“Roundness of the heart isn’t necessarily the problem per se—it’s a marker of the problem,” says co-corresponding author Shoa L. Clarke (@ShoaClarke), a preventive cardiologist and an instructor at Stanford University School of Medicine. “People with rounder hearts may have underlying cardiomyopathy or underlying dysfunction with the molecular and cellular functions of the heart muscle. It could be reasonable to ask whether there is any utility in incorporating measurements of sphericity into clinical decision-making.”
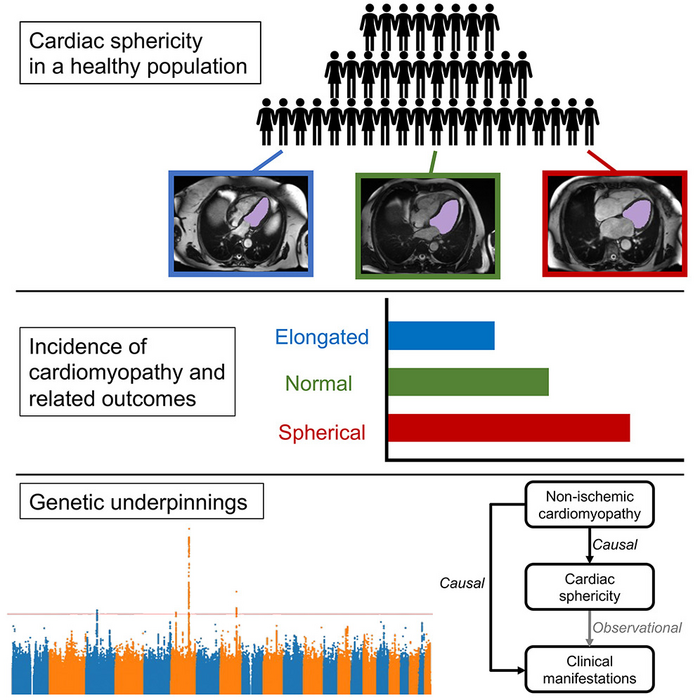
This proof-of-concept study used big data and machine learning to look at whether other anatomical changes in the heart could improve the understanding of cardiovascular risk and pathophysiology. The investigators chose to focus on sphericity because clinical experience had suggested it is associated with heart problems. Prior research had primarily focused on sphericity after the onset of heart disease, and they hypothesized that sphericity may increase even before the onset of clinical heart disease.
“We have established traditional ways of evaluating the heart, which have been important for how we diagnose and treat heart disease,” Clarke says. “Now with the ability to use deep-learning techniques to look at medical images at scale, we have the opportunity to identify new ways of evaluating the heart that maybe we haven’t considered much in the past.”
“They say a picture is worth a thousand words, and we show that this is very true for medical imaging,” says co-corresponding author David Ouyang (@David_Ouyang), a cardiologist and researcher at the Smidt Heart Institute of Cedars-Sinai. “There’s a lot more information available than what physicians are currently using. And just as we’ve previously known that a bigger heart isn’t always better, we’re learning that a rounder heart is also not better.”
This research employed data from the UK Biobank, which includes genetic and clinical information on 500,000 people. As part of that study, a subset of volunteers had MRI imaging of their hearts performed. The California-based team used data from a subset of about 38,000 UK Biobank study participants who had MRIs that were considered normal at the time of the scans. Subsequent medical records from the volunteers indicated which of them later went on to develop diseases like cardiomyopathy, atrial fibrillation, or heart failure and which did not.
The researchers then used deep-learning techniques to automate the measurement of sphericity. Increased cardiac sphericity appeared to be linked to future heart troubles.
The investigators also looked at genetic drivers for cardiac sphericity and found overlap with the genetic drivers for cardiomyopathy. Using Mendelian randomization, they were able to infer that intrinsic disease of the heart muscle—meaning defects not caused by heart attacks—caused cardiac sphericity.
“There are two ways that these findings could add value,” Ouyang says. “First, they might allow physicians to gain greater clinical intuition on how patients are likely to do at a very rapid glance. In the broader picture, this research suggests there are probably many useful measurements that clinicians still don’t understand or haven’t discovered. We hope to identify other ways to use imaging to help us predict what will happen next.”
The researchers emphasize that much more research is needed before the findings from this study can be translated to clinical practice. For one thing, the connection is still speculative and would need to be confirmed with additional data. If the link is confirmed, a threshold would need to be established to indicate what degree of sphericity might suggest that clinical interventions are needed. The team is sharing all the data from this work and making them available to other investigators to begin answering some of these questions.
Additionally, ultrasound is more commonly used than MRI to image the heart. To further advance this research, replicating these findings using ultrasound images will be useful, they note.
###
This study was supported by the National Institutes of Health.
Med, Vukadinovic et al. “Deep learning-enabled analysis of medical images identifies cardiac sphericity as an early marker of cardiomyopathy and related outcomes” https://www.cell.com/med/fulltext/S2666-6340(23)00069-7
Med (@MedCellPress), a new journal from Cell Press, publishes transformative, evidence-based science across the clinical and translational research continuum—from large-scale clinical trials to translational studies with demonstrable functional impact, offering novel insights in disease understanding. Visit https://www.cell.com/med. To receive Cell Press media alerts, please contact [email protected].
Journal
Med
DOI
10.1016/j.medj.2023.02.009
Method of Research
Observational study
Subject of Research
People
Article Title
Deep learning-enabled analysis of medical images identifies cardiac sphericity as an early marker of cardiomyopathy and related outcomes
Article Publication Date
29-Mar-2023




