In a groundbreaking fusion of bioengineering and immunology, researchers from the University of Pennsylvania’s Perelman School of Medicine and New York University’s Tandon School of Engineering have unveiled a miniature yet powerful laboratory device poised to revolutionize the future of blood cancer treatment. This “leukemia-on-a-chip” innovation promises to dramatically enhance the way chimeric antigen receptor (CAR) T cell therapies are developed and personalized, tackling the persistent challenges that have limited the efficacy of such treatments to date.
CAR T cell therapy has emerged as one of the most promising immunotherapies for blood cancers like leukemia, offering patients a tailored assault on malignant cells by reprogramming their own immune systems. Despite impressive clinical successes, a significant fraction of patients relapse, and many suffer serious adverse effects. Scientists have long grappled with the difficulty of accurately predicting patient responses or refining these therapies due to the limitations of current preclinical testing models. Conventional two-dimensional cell cultures often fail to replicate the intricate biological environments where cancer and immune cells interact, while animal models are labor-intensive, costly, and sometimes poorly predictive of human outcomes.
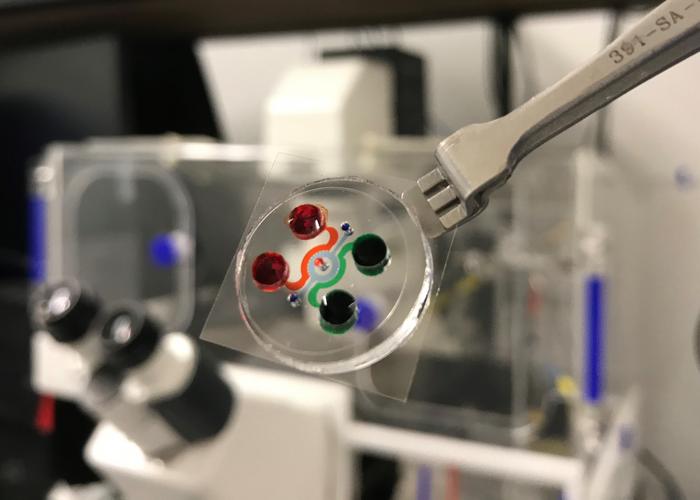
This innovative device, the size of a standard microscope slide, takes a giant leap forward by replicating the three-dimensional architecture and immunological complexity of the human bone marrow — the primary niche where leukemia cells thrive. Crucially, it incorporates not just the physical structure but also a functioning human immune system, enabling real-time observations of CAR T cell dynamics in an authentic microenvironment. The chip’s design includes three distinct bone marrow regions: blood vessels, the surrounding marrow cavity, and the outer bone lining, all populated with patient-derived bone marrow cells that self-organize and secrete key extracellular matrix components such as collagen, fibronectin, and laminin. This self-assembly recreates the native tissue architecture and its multifaceted immune ecosystem.
.adsslot_KMu5RQS6v3{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_KMu5RQS6v3{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_KMu5RQS6v3{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
The technical sophistication of this “bone marrow on a chip” permits the formation of vascularized niches that maintain realistic immune cell trafficking and interactions. This is a notable departure from traditional models that lack vascular complexity, often resulting in oversimplified or inaccurate assessments of therapeutic action. Using high-resolution imaging and advanced microscopy, the research team tracked individual CAR T cells as they navigated the microvascular networks, detected leukemia targets, and executed cytotoxic attacks. They observed with unprecedented clarity how CAR T cells slow their motility upon encountering malignant cells, facilitating direct engagement and destruction — a dynamic process previously difficult to capture in vitro or in animal models.
Beyond direct antitumor activity, the study revealed a fascinating “bystander effect,” where engineered CAR T cells stimulate non-targeted endogenous immune cells within the device. This interplay may shed light on both the therapeutic potentiation and adverse inflammatory side effects observed in patients, pointing to new avenues for modulating immune responses to maximize efficacy while minimizing toxicity. The chip also proved capable of modeling clinical scenarios including complete remission, resistance to therapy, and relapse, offering a powerful platform to study mechanisms underlying these varied outcomes.
A remarkable advantage of this platform is its scalability and time efficiency. While traditional animal models can take months to establish and require complex protocols, the leukemia-on-a-chip system can be assembled within half a day and supports experimental assays extending up to two weeks. This rapid turnaround opens the door for personalized medicine applications, where patient-specific bone marrow samples can be cultured and tested against multiple CAR T cell designs before selecting the optimal therapeutic approach.
The research team demonstrated that next-generation “fourth generation” CAR T cells, which incorporate enhanced engineering features for improved persistence and potency, outperformed earlier versions at lower dosages within the chip environment. This suggests the device’s utility in optimizing dose regimens and therapy formulations, potentially reducing toxic side effects while maintaining efficacy. Overall, this bioengineered platform represents an integrated, immunocompetent preclinical trial tool that bridges an important gap between bench research and patient care.
As regulatory agencies such as the FDA announce plans to phase out animal testing for drug safety evaluation, the timing of this breakthrough could not be more significant. By providing a physiologically relevant, animal-free model for immunotherapy testing, the leukemia-on-a-chip aligns with the drive toward humane, cost-effective, and predictive research alternatives. The device’s capacity to model dynamic, systemic immune responses within a controlled setting enables extensive mechanistic studies that can guide rational design of novel immunotherapies for leukemia and potentially other cancers.
This multidisciplinary collaboration underscores the power of combining mechanical engineering, microfluidics, cellular biology, and immunology to tackle complex challenges in cancer research. By harnessing patient-derived cells and reproducing the intricacies of the leukemia niche, researchers now have a cutting-edge tool to dissect immunotherapy resistance, identify biomarkers of response, and fine-tune treatments prior to clinical trials. The prospect that clinicians might one day leverage this technology to personalize therapy selection, improving outcomes and reducing side effects, heralds a new era in precision oncology.
The implications extend beyond leukemia alone. This platform’s modular design and ability to mimic tumor-immune interactions pave the way for similar “organ-on-a-chip” models targeting solid tumors and other hematologic malignancies. The convergence of bioengineering and immunotherapy now promises to accelerate the translation of laboratory insights into real-world cures in a timeframe and cost structure previously unimaginable.
In sum, the bioengineered leukemia-on-a-chip stands as a testament to innovation at the interface of engineering and medicine. It is poised to become a pivotal asset in the battle against cancer, not only enhancing our understanding of CAR T cell behavior in physiologically relevant contexts but also empowering clinicians and scientists to forge truly personalized treatment regimens. As this technology matures, it offers hope that the next wave of immunotherapies will be smarter, safer, and more effective, transforming lives for patients facing leukemia across the globe.
Subject of Research: Cells
Article Title: Bioengineered immunocompetent preclinical trial-on-chip tool enables screening of CAR T cell therapy for leukaemia
News Publication Date: 1-Jul-2025
Web References:
Original article DOI: 10.1038/s41551-025-01428-2
University of Pennsylvania Perelman School of Medicine: https://www.med.upenn.edu/
FDA announcement on animal testing phase-out: https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs
Image Credits: NYU Tandon Applied Micro-Bioengineering Laboratory/Courtesy of Weiqiang Chen
Keywords: Chimeric antigen receptor therapy, Blood cancer, Leukemia, Cancer treatments, Cancer immunotherapy, Biomedical engineering
Tags: bioengineering in immunologyblood cancer research breakthroughsCAR T cell therapy advancementschallenges in cancer immunotherapyimmune system reprogramming techniquesleukemia-on-a-chip technologynext-generation cancer treatment solutionsovercoming CAR T cell therapy limitationspatient response prediction in cancer therapypersonalized blood cancer treatmentpreclinical testing innovationsthree-dimensional cell culture models