Credit: University of Utah Health
Utah residents who have difficulty keeping their families fed could be missing a key ingredient: information. A University of Utah Health study finds that poor communications in at least 22 Utah communities could be hampering efforts to connect those in need with food stamps, food banks, soup kitchens, and other food resources. Researchers say the finding could help refine future community food distribution efforts.
The first-of-its-kind study, which appears in the American Journal of Preventive Medicine, pinpoints previously undetected areas in the state where a lack of information about food banks, soup kitchens, and the Supplemental Nutrition Assistance Program (SNAP)–commonly known as food stamps–is derailing efforts to alleviate food insecurity in Utah. Food insecurity is defined as the limited or uncertain availability of acquiring safe and nutritional food.
“Our findings offer a unique picture of food needs in our state that has been previously available,” says Nasser Sharareh, Ph.D., lead author of the study and a postdoctoral research associate in the Department of Population Health Sciences. “It clearly suggests that future efforts to combat food insecurity in Utah should include better use of media and other communications channels to improve awareness of referral services that help people learn more about SNAP and other emergency food providers in their communities.”
About one in eight households in Utah struggle to provide food for their families, according to the Food & Research Action Center, a national anti-hunger advocacy group. In October 2019, more than 165,000 Utahans participated in SNAP, according to the U.S. Department of Agriculture.
In the past, accessibility or availability of food resources, such as grocery stores, and the ability of individuals or households to buy that food were two key measures of food insecurity. However, these traditional indicators may not fully reflect the scope of the problem.
To determine what role information–or the lack of it–has on requests for food assistance in the state, Sharareh and his colleagues tracked SNAP enrollment in 99 Utah communities for a year. Then, they correlated that data with food information requests received from those communities by United Way 211 (UW211), a nonprofit emergency services referral hotline.
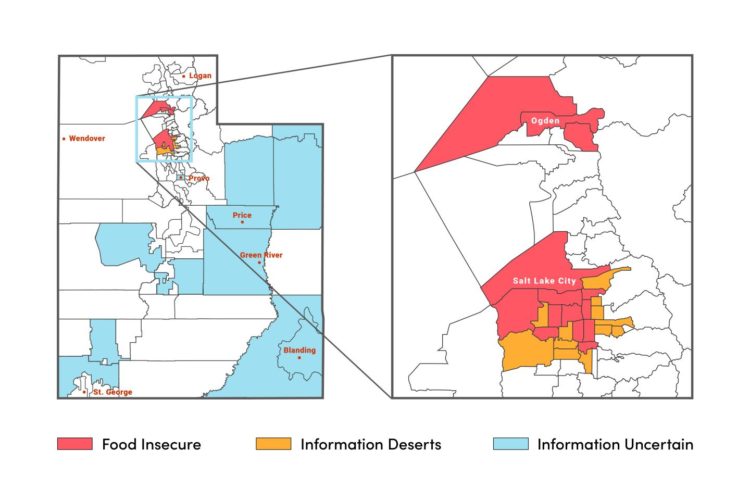
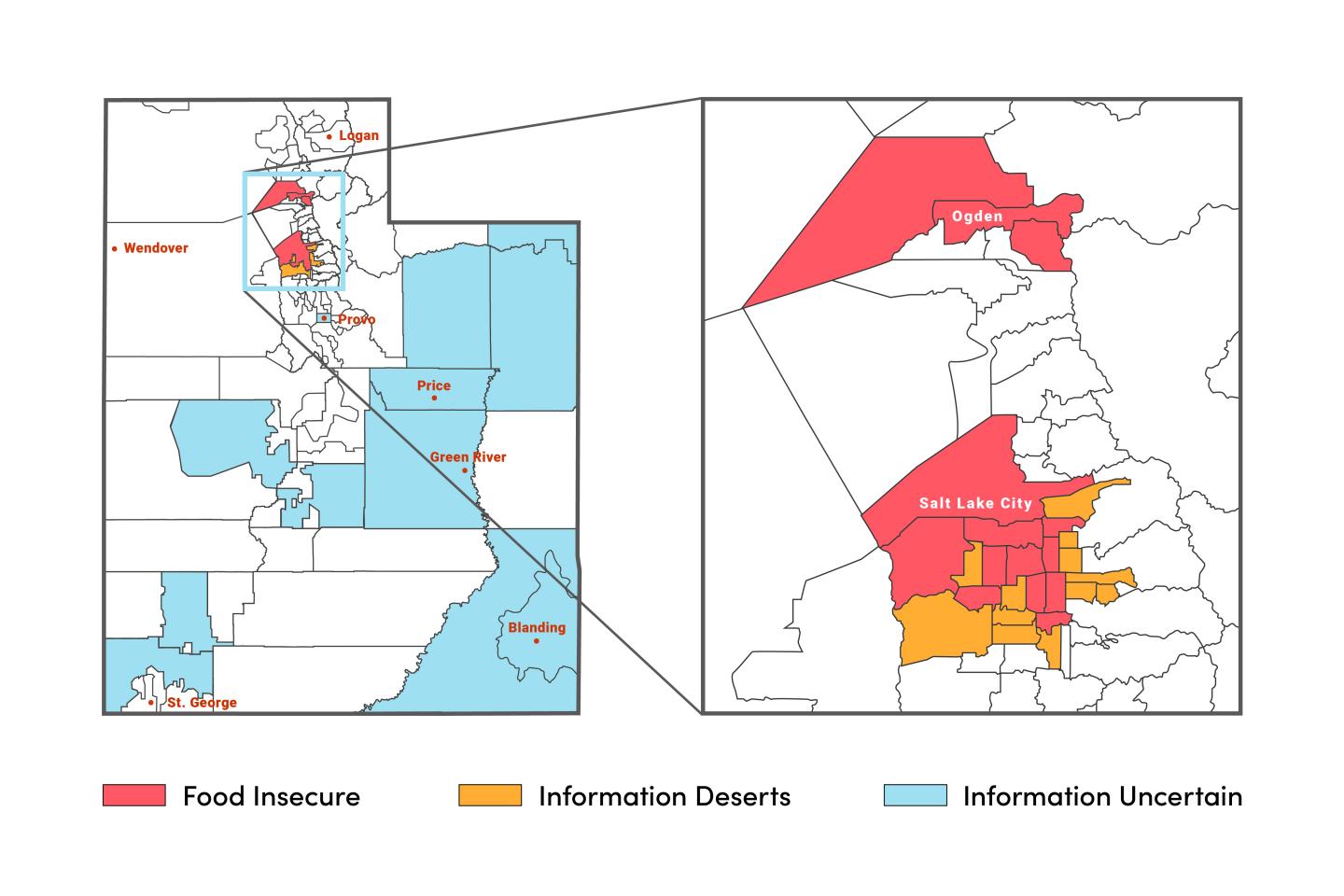
Using data analysis and a geographic information system (GIS) method, the researchers identified four clusters of communities (total number in parenthesis).
- Food Secure (63) – SNAP enrollment and UW211 call rates are both low. Residents likely have little or no need for food assistance programs or information about them. These areas include Park City, St. George, Morgan, and Weber County.
- Food Insecure (14) – SNAP enrollment and UW211 call rates are high; residents are in great need of food assistance programs and information about them. These areas include downtown Salt Lake City, Rose Park, and Glendale.
- Information Deserts (11) ¬- Low SNAP enrollment but high rate of UW211 calls. Residents might not be aware of SNAP and have little or no knowledge of other community food resources. In these “deserts,” UW211 serves as a vital “oasis,” referring information-starved callers to community food resources that they were previously unaware of. Areas include Sugar House, The Avenues, Holladay, and West Jordan.
- Information Uncertain (11) – High SNAP participation and low rate of UW211 calls. Residents use SNAP but might not be aware of UW211. SNAP alone might be meeting their existing needs. These areas include Carbon, Emery, and San Juan Counties.
The researchers will continue tracking how information availability influences requests for food assistance, particularly in the 22 newly identified information deserts and information uncertain communities that are at high risk of becoming food insecure in the future. In the meantime, the scientists hope their research helps inform public policy decisions regarding food assistance.
“This study offers emergency food providers with a snapshot of where their services are most needed and why they need to bolster their efforts to get timely and reliable information into the hands of those seeking their help,” says Andrea Wallace, Ph.D., R.N., the study’s senior author and chair of health systems and community-based care in the College of Nursing. “It could lead to policies that help communities better serve residents in need of food assistance, now and in the future.”
Based on these findings, the researchers plan to expand their work to identify at-risk communities in more than 15 other states.
In the current study, 36 Utah regions, communities, and neighborhoods were designated as food insecure, information deserts, or information uncertain. They are:
Food Insecure: Ben Lomond, Kearns, Manga, Midvale, Murray, Ogden (downtown), Salt Lake City (downtown, Glendale, Rose Park), South Ogden, South Salt Lake, Taylorsville (east)/Murray (west), West Valley (center), West Valley (east).
Information Deserts: Holladay, Millcreek (south), Sandy, Salt Lake City (The Avenues, Southeast Liberty, Sugar House), Taylorsville (west), West Jordan (northeast, southeast, west/Copperton), West Valley (west).
Information Uncertain: Blanding/Monticello, Carbon County, Cedar City, Daggett and Uintah County, Delta/Fillmore, Emery County, Provo (west city center), Richfield/Monroe/Salina, San Juan County, Washington County.
###
In addition to Drs. Sharareh and Wallace, Drs. Rachel Hess, Neng Wan, and Cathleen Zick contributed to this study. Dr. Sharareh conducted this work through a contract with United Way of Salt Lake.
University of Utah Health provides leading-edge and compassionate medicine for a referral area that encompasses 10% of the U.S., including Idaho, Wyoming, Montana, and much of Nevada. A hub for health sciences research and education in the region, U of U Health touts a $356 million research enterprise and trains the majority of Utah’s physicians and more than 1,250 health care providers each year at its Schools of Medicine and Dentistry and Colleges of Nursing, Pharmacy, and Health. With more than 20,000 employees, the system includes 12 community clinics and four hospitals. For 10 straight years, U of U Health has ranked among the top 10 U.S. academic medical centers in the rigorous Vizient Quality and Accountability Study, including reaching No. 1 in 2010 and 2016.
Media Contact
Doug Dollemore
[email protected]
801-587-2596