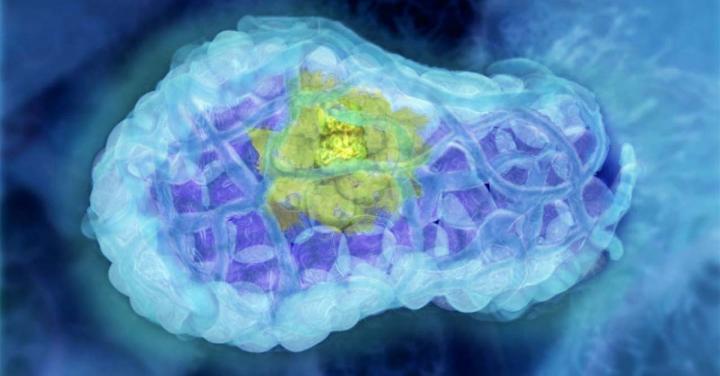
Credit: Walter and Eliza Hall Institute, Australia
The anti-cancer medicine venetoclax could improve the current therapy for estrogen receptor-positive (ER+) breast cancer – the most common form of breast cancer in Australia – according to preclinical studies led by Walter and Eliza Hall Institute researchers.
The research team showed that venetoclax could kill breast cancer cells that had been ‘put to sleep’ by a drug that blocks cell division (called a CDK4/6 inhibitor), which is currently used in combination with hormone therapies to treat ER+ breast cancer. The research, which used breast cancer cells taken from patients, was the first to show that venetoclax could kill sleeping, or ‘senescent’, cancer cells.
The promising preclinical results for this ‘triple therapy’ have underpinned a phase 1 clinical trial in Melbourne that is combining venetoclax with hormone therapy and CDK4/6 inhibitors in patients with ER+ breast cancer.
Dr James Whittle, Professor Geoff Lindeman and Professor Jane Visvader led the research, which was published in Clinical Cancer Research.
At a glance
- ER+ breast cancers are currently treated with a combination of a hormone therapy plus a CDK4/6 inhibitor drug. These force the cancer cells into a ‘sleeping’ state but do not kill them, leading to a high risk of eventual cancer relapse.
- Using hormone receptor-positive breast cancer samples taken from patients, our researchers showed that adding the anti-cancer drug venetoclax to the hormone therapy/CDK4/6 inhibitor combination could kill the ‘sleeping cells’ – potentially prolonging the cancer’s response to therapy.
- The potential new ‘triple therapy’ for hormone receptor-positive breast cancer is now being assessed in a phase 1 clinical trial in Melbourne.
Killing sleeping cells
Around 70 per cent of breast cancer cases in Australia are estrogen-receptor positive, meaning they will grow in response to the female hormone estrogen. The current ‘gold standard’ therapy for treating these breast cancers on relapse is a combination of anti-hormone therapy – which prevents estrogen signalling – plus a medicine called a CDK4/6 inhibitor that blocks cell division, said Dr James Whittle, a clinician PhD student at the Institute and a medical oncologist at the Peter MacCallum Cancer Centre.
“This current therapy works well in slowing cancer growth, but it does not actually kill the cancer cells – it just sends them into a sleeping or dormant state, called senescence,” he said. “This unfortunately means cancer relapse is virtually inevitable. In fact, the majority of breast cancer deaths in Australia are from patients with ER+ breast cancer.
“If we could find a way to kill these sleeping cancer cells, we might be able to help patients live longer. To do this, we looked to medicines that directly block the proteins that help cancer cells to survive,” he said.
The team examined whether ER+ breast cancer cells were sensitive to venetoclax, an anti-cancer medicine that inhibits the cell survival protein BCL-2. Venetoclax is in clinical use for treating certain types of blood cancers, and in clinical trials for a range of cancers including breast cancer.
“We discovered that venetoclax could indeed kill ER+ breast cancer cells that had been treated with a CDK4/6 inhibitor – even those that were senescent. This was an exciting result as it was the first time that venetoclax has been shown to kill senescent cells,” Dr Whittle said.
Triple therapy threat for tumours
In several laboratory models, including those using ER+ breast cancer samples from patients, the researchers showed that adding venetoclax to the combination of hormone therapy and a CDK4/6 inhibitor led to a better and longer-term response of the tumour to the therapy, said Professor Lindeman, who is a clinician-scientist at the Institute and a medical oncologist at the Peter MacCallum Cancer Centre.
“These promising results provided a justification for starting clinical trials to look at a ‘triple therapy’ combining venetoclax, hormone therapy and a CDK4/6 inhibitor in patients with ER+ breast cancer,” Professor Lindeman said.
“We have initiated the phase 1 PALVEN trial which will, in the first place, look at whether this triple therapy is safe for patients, and will also consider how patients’ tumours respond to the triple therapy.
“It would be wonderful to see a new therapy that improves the outcomes of patients with ER+ breast cancer,” Professor Lindeman said.
(Due to COVID-19, the PALVEN trial is currently not accepting new participants).
###
Venetoclax was developed by AbbVie and Genentech, a member of the Roche Group, in collaboration with Walter and Eliza Hall Institute scientists.
The research was supported by the Australian National Health and Medical Research Council, the Australian Cancer Research Foundation, National Breast Cancer Foundation, Breast Cancer Research Foundation, Qualtrough Cancer Research Fund, Joan Marshall Breast Cancer Research Fund, Tracey Keogh and Sharon Croft, Collie Foundation, Royal Australasian College of Physicians, Cancer Council Victoria and the Victorian Government. Breast cancer samples were provided by the Victorian Cancer Biobank. Dr Whittle is PhD student at the Institute, enrolled through the University of Melbourne’s Department of Medical Biology.
Media Contact
Vanessa Solomon
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




