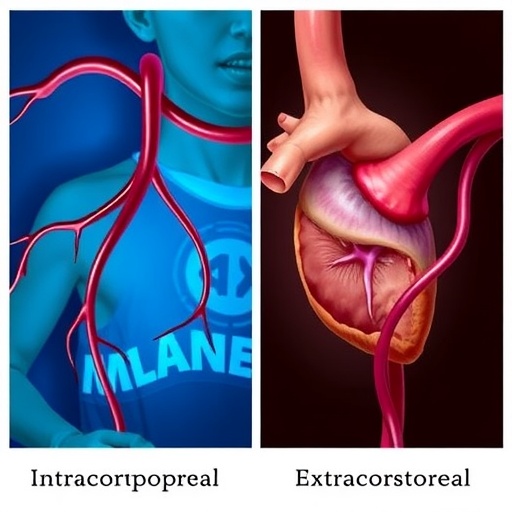
In the evolving realm of minimally invasive surgical oncology, a pivotal clinical investigation is underway in Japan that stands to redefine colorectal cancer treatment paradigms. The INEX study, a large-scale, multicenter randomized controlled trial (RCT), embarks on an important comparative journey to evaluate the long-term outcomes of intracorporeal anastomosis (IA) versus extracorporeal anastomosis (EA) in patients with stage II and III colon cancer. This landmark research addresses unresolved questions about the oncological safety and effectiveness of two surgical techniques amid increasing adoption of advanced laparoscopy and robot-assisted procedures.
Minimally invasive surgery has revolutionized the management of colorectal cancer, aiming to reduce patient morbidity without compromising oncological integrity. Intracorporeal anastomosis, where the reconnection of bowel segments is performed entirely within the abdominal cavity, has piqued interest due to smaller incisions, less postoperative pain, and expedited recovery. However, despite its growing popularity, clinical confidence in IA’s long-term oncological equivalence to the traditional extracorporeal approach remains tentative, fueled by theoretical concerns about tumor cell spread due to bowel manipulation under elevated intra-abdominal pressures.
Addressing this clinical equipoise, the INEX trial meticulously plans to enroll 1,400 patients diagnosed with clinical stage II or III colon cancer scheduled for laparoscopic or robot-assisted colectomy. Participants, drawn from 47 tertiary institutions throughout Japan, will be randomized to undergo either IA or EA. This rigorous trial design ensures broad applicability across varied practice settings while maintaining surgical quality through mandatory inclusion of board-certified endoscopic surgeons at each site.
.adsslot_7LcSYi921y{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_7LcSYi921y{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_7LcSYi921y{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Colon tumors eligible for inclusion are located in the cecum, ascending colon, transverse colon, or descending colon, reflecting a comprehensive coverage of typical colorectal cancer sites amenable to minimally invasive surgery. Each surgical intervention follows stringent oncological principles, with D2 or D3 lymph node dissection performed per the Japanese Classification of Colorectal Carcinoma, guaranteeing that cancer clearance standards remain uncompromised irrespective of the anastomosis technique employed.
The principal focus of the trial is the primary endpoint of relapse-free survival (RFS), a robust oncological outcome measure encompassing recurrence rates and disease progression. Long-term follow-up is integral to this study, enabling clinicians and researchers to discern subtle differences in cancer control that short-term studies might miss, especially in addressing concerns about peritoneal dissemination believed to be associated with intracorporeal techniques.
From a technical vantage, intracorporeal anastomosis leverages refined laparoscopic or robotic instruments to reconstruct the bowel entirely inside the abdomen, minimizing external bowel manipulation. This contrasts with extracorporeal anastomosis, which necessitates exteriorizing the bowel segments through an abdominal incision for anastomosis—potentially resulting in larger incisions and increased tissue trauma. The IA method’s potential to mitigate incision size has translated into observable reductions in postoperative pain, faster gastrointestinal recovery, and shorter hospital stays in preliminary studies.
Nevertheless, basic science insights urge caution. During IA, high intra-abdominal pressure from pneumoperitoneum and manipulation of the intestinal lumen may theoretically facilitate tumor cell shedding into the peritoneal cavity, increasing risks for peritoneal recurrence—an oncologically devastating outcome. Existing literature on this phenomenon is limited, largely comprising retrospective analyses or small cohort studies, thereby underscoring the pressing need for a definitive RCT.
Current clinical guidelines worldwide do not explicitly favor IA over EA due to insufficient high-quality evidence, leading many surgeons to select the anastomotic technique based on personal expertise and institutional resources. The INEX study promises to fill this knowledge gap by providing rigorous, prospective data and potentially endorsing evidence-based standards that align surgical approach with oncological safety and patient recovery benefits.
The operationalization of this trial exemplifies collaborative surgical oncology research, uniting leading colorectal surgery centers with expertise in minimally invasive techniques. Comprehensive quality controls—such as surgeon certification requirements and uniform procedural standards—ensure consistency and reliability of outcomes, which will be critically analyzed upon trial completion.
Should IA prove non-inferior to EA in relapse-free survival, the implications are profound. Patients could benefit from less invasive procedures without compromising cancer control, while healthcare systems might see enhanced throughput and reduced postoperative complications. Moreover, the confirmation of IA’s oncological safety could drive guideline updates, harmonizing surgical protocols globally and stimulating further innovation in robot-assisted colorectal surgery.
Conversely, if intracorporeal anastomosis fails to demonstrate comparable long-term oncological outcomes, the trial will cement the status of extracorporeal anastomosis as the gold standard, safeguarding patients against potentially higher recurrence risks. This evidence-based clarity will refocus surgical training and institutional practices, ensuring patient safety remains paramount.
The INEX trial also paves the way for future research avenues, including investigations into molecular biomarkers predicting recurrence risks related to surgical techniques, or integration of intraoperative imaging modalities to minimize tumor cell spillage. Additionally, it will offer rich data for health economists analyzing cost-effectiveness between IA and EA within different healthcare paradigms.
Clinicians, researchers, and patients alike eagerly anticipate the results of this pivotal study, which carries the potential to transform colorectal cancer surgery substantially. By clarifying whether the technical advancements of intracorporeal anastomosis translate into durable oncological outcomes, the INEX trial champions precision medicine’s spirit, marrying innovative surgical techniques with evidence-based clinical decision-making.
In this era of personalized cancer care, where minimizing treatment morbidity without sacrificing efficacy is the holy grail, the ongoing comparison between intracorporeal and extracorporeal anastomosis embodies an essential quest. The Japanese multicenter collaboration powering the INEX study sets a new standard for integrating surgical innovation with rigorous scientific inquiry, aiming ultimately to enhance survival and quality of life for patients confronting colon cancer worldwide.
As the surgical community awaits the culmination of this trial, the broader oncology field stands to gain critical insights about balancing cutting-edge techniques with long-term safety—a reminder that progress in cancer treatment must always be carefully measured, patient-centered, and grounded in solid evidence.
Subject of Research: Comparison of long-term oncological outcomes between intracorporeal and extracorporeal anastomosis techniques in stage II/III colon cancer surgery.
Article Title: Long-term prognosis of intracorporeal versus extracorporeal anastomosis in stage II/III colorectal cancer (INEX study): study protocol for a multicenter randomized controlled trial in Japan.
Article References:
Hanaoka, M., Kagawa, H., Ishiguro, M. et al. Long-term prognosis of intracorporeal versus extracorporeal anastomosis in stage II/III colorectal cancer (INEX study): study protocol for a multicenter randomized controlled trial in Japan. BMC Cancer 25, 1242 (2025). https://doi.org/10.1186/s12885-025-14676-x
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14676-x
Tags: bowel resection methods efficacyclinical trial on colon cancer surgeryextracorporeal anastomosis comparison studyINEX trial colorectal cancer outcomesintracorporeal anastomosis in colorectal surgerylaparoscopic colectomy techniqueslong-term outcomes of anastomosis methodsminimally invasive surgical oncology researchoncological safety of surgical techniquespostoperative recovery in anastomosisrobot-assisted surgery in cancer treatmentstage II and III colon cancer treatment