Credit: UPMC, created with BioRender.com
PITTSBURGH, Feb. 15, 2021 – A paper published today in Nature shows how chemicals in the areas surrounding tumors–known as the tumor microenvironment–subvert the immune system and enable cancer to evade attack. These findings suggest that an existing drug could boost cancer immunotherapy.
The study was conducted by a team of scientists at UPMC Hillman Cancer Center and the University of Pittsburgh School of Medicine, led by Greg Delgoffe, Ph.D., Pitt associate professor of immunology. By disrupting the effect of the tumor microenvironment on immune cells in mice, the researchers were able to shrink tumors, prolong survival and increase sensitivity to immunotherapy.
“The majority of people don’t respond to immunotherapy,” said Delgoffe. “The reason is that we don’t really understand how the immune system is regulated within this altered tumor microenvironment.”
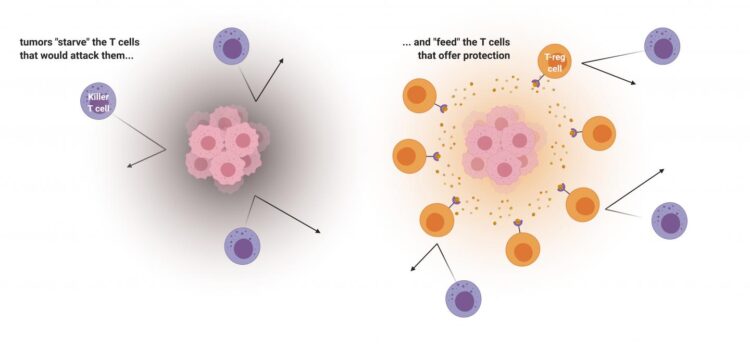
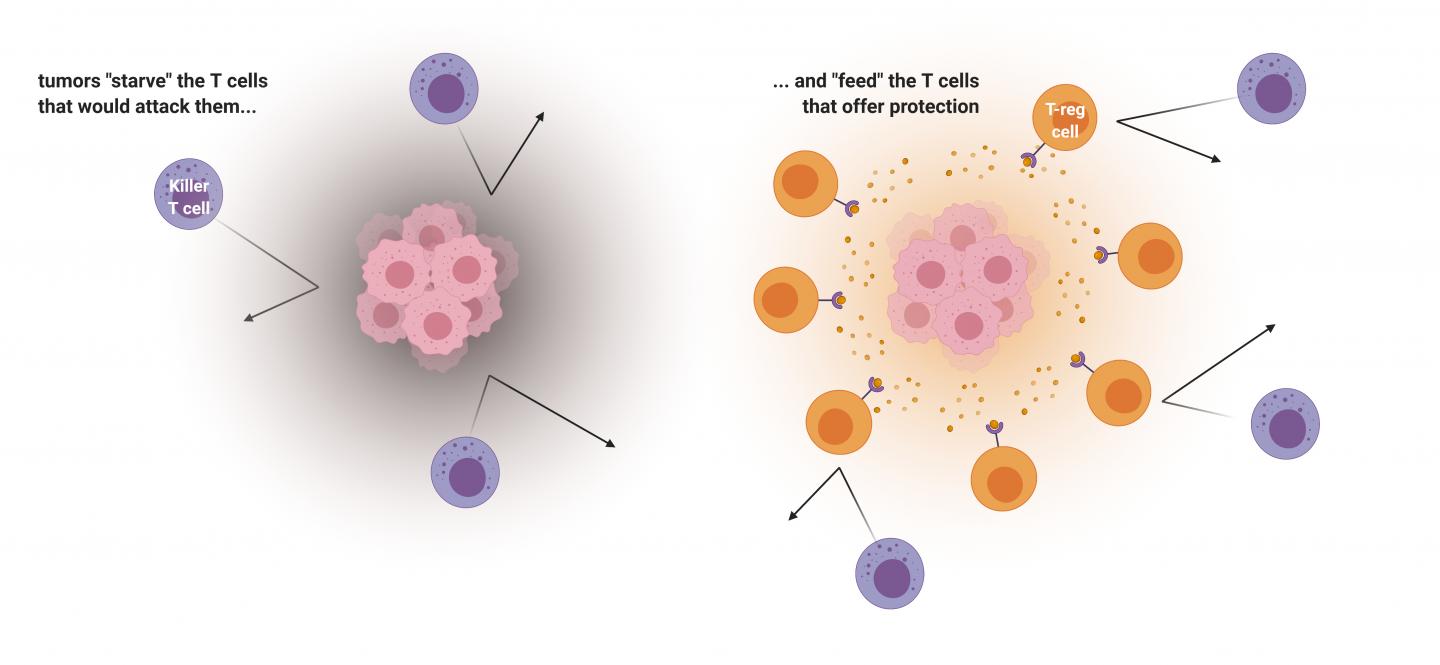
The immune system is made up of many kinds of cells, chief among them T cells. One type, called killer T cells, fights off invaders, such as viruses, bacteria and even cancer. Another type, called regulatory T cells, or “T-reg cells” for short, counteracts killer T cells by acting as protectors of the cells that belong to the body. T-reg cells are important for preventing autoimmune diseases, such as type I diabetes, Crohn’s disease and multiple sclerosis, where overactive killer T cells assault the body’s healthy tissues.
For all of these different immune cells to do their jobs, they need to produce energy. Delgoffe’s team studied how these different types of T cells have different appetites, and how tumors–which have large appetites–compete for nutrients with infiltrating immune cells. The researchers found that killer T cells and regulatory T cells have very different appetites, and cancer cells exploit this.
“Cancer is wise to the whole situation,” Delgoffe said. “Cancer cells don’t just starve T cells that would kill them but actually feed these regulatory T cells that would protect them.”
In short, Delgoffe’s team found that tumors gobble up all the vital nutrients in their vicinity that killer T cells would need to attack. Further, they also excrete lactic acid, which feeds the regulatory T cells, convincing them to stand guard. T-regs can turn the lactic acid into energy, using a protein called MCT1, so nuzzling up with the tumor is a good way for these immune cells to stay fed.
“What better way to recruit a cell than food?” Delgoffe said.
Then, using mice with melanoma, the researchers found that silencing the gene that codes for the MCT1 protein caused tumor growth to slow down. The mice also lived longer.
“We starved the T-regs,” said Delgoffe. “When T-reg cells are not being sustained by the tumor, killer T cells can come in and kill the cancer.”
Importantly, when Delgoffe’s team combined MCT1 inhibition with immunotherapy, the anti-cancer effects were stronger than either strategy alone.
Clinically, the same effect might be achievable using drugs that inhibit MCT1–one of which is currently being tested in people with advanced lymphoma, and it appears to be well-tolerated.
###
Additional authors on the study include McLane Watson, Paolo Vignali, Steven Mullett, Abigail Overacre-Delgoffe, Ph.D., Ronal Peralta, Stephanie Grebinoski, Ashley Menk, Natalie Rittenhouse, Kristin DePeaux, Ryan Whetstone, Ph.D., Dario Vignali, Ph.D., Timothy Hand, Ph.D., Amanda Poholek, Ph.D., and Stacy Wendell, Ph.D., of Pitt and UPMC; and Brett Morrison, M.D., Ph.D., and Jeffrey Rothstein, M.D., Ph.D., of Johns Hopkins University.
Funding for this study was provided by the Sidney Kimmel Foundation, National Institutes of Health (DP2AI136598, P50CA121973, P50CA097190 R01DK089125, R01CA203689, P01AI108545, T32CA082084, F31AI149971, F30CA247034, F31CA247129, T32AI089443 and F31AI147638), the American Association for Cancer Research (SU2CAACR-IRG-04-16), the Alliance for Cancer Gene Therapy, the Mark Foundation for Cancer Research, Cancer Research Institute, the Sy Holzer Endowed Immunotherapy Fund and the Damon Runyon Cancer Research Foundation.
Additional Contact:
Cyndy Patton
Mobile: 412-415-6085
E-mail: [email protected]
About UPMC Hillman Cancer Center
UPMC Hillman Cancer Center, ranked 7th by U.S. News & World Report in 2019 for excellence in cancer care, is the region’s only National Cancer Institute-designated Comprehensive Cancer Center and is one of the largest integrated community cancer networks in the United States. Backed by the collective strength of UPMC and the University of Pittsburgh School of Medicine, UPMC Hillman Cancer Center has nearly 70 locations throughout Pennsylvania and Ohio with cancer centers and partnerships internationally. The more than 2,000 physicians, researchers and staff are leaders in molecular and cellular cancer biology, cancer immunology, cancer virology, biobehavioral oncology, and cancer epidemiology, prevention, and therapeutics. UPMC Hillman Cancer Center is transforming cancer research, care, and prevention — one patient at a time.
About the University of Pittsburgh School of Medicine
As one of the nation’s leading academic centers for biomedical research, the University of Pittsburgh School of Medicine integrates advanced technology with basic science across a broad range of disciplines in a continuous quest to harness the power of new knowledge and improve the human condition. Driven mainly by the School of Medicine and its affiliates, Pitt has ranked among the top 10 recipients of funding from the National Institutes of Health since 1998. In rankings recently released by the National Science Foundation, Pitt ranked fifth among all American universities in total federal science and engineering research and development support.
Likewise, the School of Medicine is equally committed to advancing the quality and strength of its medical and graduate education programs, for which it is recognized as an innovative leader, and to training highly skilled, compassionate clinicians and creative scientists well-equipped to engage in world-class research. The School of Medicine is the academic partner of UPMC, which has collaborated with the University to raise the standard of medical excellence in Pittsburgh and to position health care as a driving force behind the region’s economy. For more information about the School of Medicine, see http://www.
http://www.
To read this release online or share it, visit https:/
Media Contact
Erin Hare
[email protected]