Cancer immunotherapy has revolutionized the treatment landscape for several malignancies by mobilizing the adaptive immune system, particularly T cells, to recognize and eliminate cancer cells. Despite its success in certain cancers such as melanoma, lung, and hematologic malignancies, its efficacy remains disappointingly limited against solid tumors. These tumors frequently establish immunologically “cold” microenvironments, characterized by a lack of active immune infiltration and suppressed anti-tumor immune functions, making them difficult targets for conventional immunotherapies. Overcoming this challenge requires innovative approaches that can effectively awaken dormant immune pathways in these refractory tumor niches.
Enter Lingyin Li, PhD, a biochemist and professor at Stanford University’s Department of Biochemistry and the ChEM-H institute, whose groundbreaking work explores a novel immunotherapeutic strategy aimed at converting these “cold” solid tumors into “hot,” immunologically active ones. Unlike traditional immunotherapies that primarily stimulate the adaptive immune response, Dr. Li’s approach harnesses a powerful mechanism of the innate immune system centered on the small molecule cyclic GMP-AMP (cGAMP). As a rapid responder to cellular damage and pathogenic threats, cGAMP triggers immediate inflammatory signaling through the STING (stimulator of interferon genes) pathway, acting as a first line of defense.
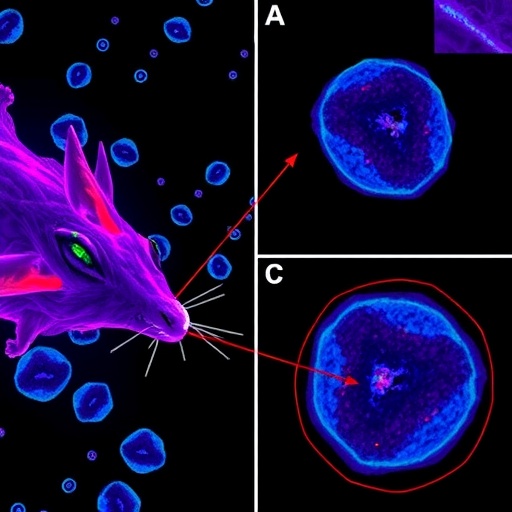
One of the pivotal discoveries made by Li’s lab unveiled that tumors evade immune surveillance not only by silencing adaptive immunity but also by actively degrading cGAMP through overexpression of the enzyme ectonucleotide pyrophosphatase/phosphodiesterase 1 (ENPP1). ENPP1 catalyzes the hydrolysis of extracellular cGAMP, effectively preventing it from activating STING pathways in surrounding immune cells. This degradation maintains the tumor’s cold microenvironment, allowing malignant cells to proliferate unchecked. Understanding this molecular camouflage mechanism framed the hypothesis that inhibiting ENPP1 could bolster innate immune signaling within tumors and enhance anti-cancer immunity.
Capitalizing on this insight, Dr. Li and her interdisciplinary team synthesized STF-1623, a potent and selective small-molecule inhibitor of ENPP1. This drug is designed to specifically bind to and block ENPP1 activity localized on the tumor cell surface, thereby preserving cGAMP levels within the tumor microenvironment. Their recent publication in Cell Reports Medicine (September 2025) provides compelling preclinical evidence that STF-1623 amplifies intratumoral cGAMP concentrations, which in turn activate the STING pathway in immune cells, transforming inert tumors into hotbeds of immunological activity.
In meticulous in vivo studies employing multiple mouse models—covering breast, pancreatic, colorectal, and glioblastoma cancers—STF-1623 demonstrably suppressed tumor growth without eliciting detectable adverse effects. This selective safety profile results from the drug’s mechanism of targeting ENPP1, which is highly concentrated on tumor cells but expressed at minimal levels in healthy tissues. Consequently, STF-1623 primarily acts where it is needed, mitigating systemic inflammation and associated toxicities often observed with broader immune activators.
At the molecular level, structural biology elucidated the intimate interaction between STF-1623 and ENPP1. The inhibitor occupies the enzyme’s active site, coordinating with essential zinc ions and displaying long-term binding affinity exceeding 24 hours. This durable engagement potentiates sustained inhibition of cGAMP hydrolysis, thus amplifying the persistence of cGAMP signaling in the tumor milieu. This mechanism sets STF-1623 apart from conventional STING agonists, which attempt to directly stimulate the pathway, often resulting in unrestrained inflammation and limited clinical success.
Moreover, STF-1623’s mode of action leverages endogenous cGAMP produced by cancer cells in response to genomic instability—a hallmark of tumors characterized by DNA damage and mutation burden. Cytosolic DNA leaks from the nucleus or mitochondria activate the DNA sensor cGAS, catalyzing cGAMP synthesis. However, cancer cells exploit ENPP1 to evade this innate alert system, thereby dampening immune activation. By neutralizing ENPP1, STF-1623 reinstates this ancient surveillance checkpoint, mobilizing innate immune effectors including type I interferons, dendritic cells, and natural killer cells to mount a robust anti-tumor assault.
Despite the promise of STF-1623 as a monotherapy, Dr. Li emphasizes that the inherent complexity of cancer necessitates combination strategies. Preclinical data indicate enhanced efficacy when STF-1623 is administered alongside other cancer therapies such as checkpoint inhibitors or chemotherapies. This combinatorial approach may synergistically unmask tumors to immune detection, improve infiltration of cytotoxic lymphocytes, and overcome resistance mechanisms. Such targeted activation of innate immunity at the tumor site could complement the systemic adaptive immune engagement fostered by existing immunotherapies.
Another notable advantage of STF-1623 arises from its ability to finely tune the immune response by preserving physiological cGAMP signaling, rather than artificially activating STING with synthetic agonists. This nuanced modulation of innate immunity is expected to reduce off-target effects and excessive inflammation that have plagued early clinical trials with direct STING agonists. By working with the body’s natural defense mechanisms, STF-1623 represents a paradigm shift in designing immunotherapies that precisely recalibrate tumor-immune interactions.
With promising preclinical efficacy and an encouraging safety profile, STF-1623 has recently obtained FDA clearance to initiate Phase I clinical trials. Patient enrollment is anticipated to commence shortly, marking a significant milestone in the translation of innate immune checkpoint blockade from bench to bedside. These clinical studies will critically evaluate the drug’s safety, pharmacokinetics, and preliminary anti-cancer activity in humans, laying the groundwork for potential new treatment avenues for patients with cancers unresponsive to current immunotherapies.
Dr. Li’s pioneering work at the Arc Institute, an independent nonprofit dedicated to accelerating biomedical discovery through collaborative and curiosity-driven research, exemplifies the transformative potential of innovative immune-targeted drug design. Supported by both public and private funders such as the National Institutes of Health and Angarus Therapeutics, this research integrates structural biology, immunology, and translational science to confront one of oncology’s most stubborn challenges: treating the invisible, immune-evading cold tumors.
As the field moves forward, the success of STF-1623 could inspire a broader class of innate immune checkpoint inhibitors, expanding the therapeutic arsenal against solid tumors. By illuminating the intricate crosstalk between cancer cells and the innate immune system, Dr. Li’s research ushers in a new era—one where the body’s first responders are empowered to rally a powerful, localized immune offense against elusive malignancies.
Subject of Research: Animals
Article Title: Innate immune checkpoint blockade with an ENPP1 inhibitor boosts intratumoral cGAMP to drive anti-cancer immunity
News Publication Date: 5-Sep-2025
Web References:
https://www.cell.com/cell-reports-medicine/fulltext/S2666-3791(25)00409-4
References:
Wang S., Johnson R., Carozza J., Fernandez D., Scicinski J., Verity N., Mardjuki R., Cao X., Guo Y., Papkoff J., Ray N., Li L. (2025). Innate immune checkpoint blockade with an ENPP1 inhibitor boosts intratumoral cGAMP to drive anti-cancer immunity. Cell Reports Medicine. DOI: 10.1016/j.xcrm.2025.102336
Image Credits: Raymond Rudolph
Keywords: Cancer, Biomedical engineering, Drug design
Tags: biochemistry of cancer immunotherapycancer immunotherapy advancementscyclic GMP-AMP therapeutic strategyimmunologically active tumor microenvironmentsinnate immune checkpoint inhibitorsinnovative cancer treatment approachesnovel treatments for solid tumorsovercoming immunotherapy resistancesolid tumor immunotherapyStanford University cancer researchSTING pathway activation in cancerTransforming cold tumors to hot tumors